More Information
Submitted: December 04, 2023 | Approved: December 19, 2023 | Published: December 20, 2023
How to cite this article: Govani DJ, Zaparackaite I, Singh SJ, Bhattacharya D, Swamy KB, et al. An Innovative Therapy by Changing the Gut Microbiome for the Dual Post-Operative Complications of the Recurrent Methicillin-Resistant Staphylococcus aureus (MRSA) Infections in the Residual Type II First Branchial Cyst and Facial Nerve Palsy. Heighpubs Otolaryngol Rhinol. 2023; 7: 005-011.
DOI: 10.29328/journal.hor.1001027
Copyright License: © 2023 Govani DJ, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Bowel motility disorders; Branchial anomalies; Branchial cyst; Branchial fistula; Branchial sinus; Cervical abscess; Cervical sinus; Facial nerve palsy; Hypoganglionosis; MRSA; Parotid preservation
An Innovative Therapy by Changing the Gut Microbiome for the Dual Post-Operative Complications of the Recurrent Methicillin-Resistant Staphylococcus aureus (MRSA) Infections in the Residual Type II First Branchial Cyst and Facial Nerve Palsy
Govani DJ1, Zaparackaite I2, Singh SJ3, Bhattacharya D4, Swamy KB5, Correia RC6, Midha PK7 and Patel RV8*
1Medical Student, B J Med College and New Civil Hospital, Ahmedabad, Gujarat, India
2Department of Pediatric Surgery, Emergency’s Children’s Surg Hosp, Entebbe/ Evelina Children’s Hosp, London, UK
3Department of Pediatric Surgery, Nottingham University Hospitals, Nottingham, UK
4Department of Pediatric Surgery, Sultan Qaboos Hospital, Salalah, Sultanate of Oman
5Lincoln University College, Lincoln University, Kuala Lumpur, Malaysia
6Santa Casa de Tatui Gen Hospital, 330 Maneco Pereira Road, Tatui 18273000, Sao Paulo, Brazil
7J. Watumull Global Hospital & Research Centre, Delwara Road, Mount Abu, Rajasthan, Affiliated to Medical Faculty of God Fatherly World Spiritual University, Mount Abu, Rajasthan, India
8Departments of Pediatrics and Pediatric Surgery, Postgraduate Institute of Child Health & Research and KT Children Government University Teaching Hospital, Rajkot 360001, Gujarat, India
*Address for Correspondence: Patel RV, MD, MS, MCh, LL M, DCH, DNBPS, FRCSEd, FRCS Ped, FEBPS, FACS, FAAP, Director-Professor, Departments of Pediatrics and Pediatric Surgery, Postgraduate Institute of Child Health & Research and KT Children Government University Teaching Hospital, Rajkot 360001, Gujarat, India, Email: [email protected]
A very unusual, interesting, and challenging case of a 24-year-old female who was born with three openings in the neck. The patient had chronic abdominal gaseous distention, recurrent abdominal pain, and constipation since early infancy. The patient presented in emergency with acute painful red, hot, and tender swelling in the left upper cervical area. Laboratory studies showed high inflammatory markers and a provisional diagnosis of abscess with a sinus was made. The patient underwent an emergency incision and drainage. Sinus recurred and a sinogram showed it to be a residual cyst in the left submandibular salivary gland. The total cyst excision was attempted with resultant recurrence and grade IV facial nerve palsy. Post-operatively recurrent infections caused by Methicillin-resistant Staphylococcus aureus (MRSA) required several courses of oral and intravenous broad-spectrum antibiotics with several hospital admissions with no resolution in sight. Subsequent ultrasound and magnetic resonance imaging showed a residual infected cyst, cutaneous sinus, and a fistula opening in the left ear canal. A diagnosis of branchial cyst type II of the first brachial cleft remnant with a fistula was established with bilateral branchial fistulas of the second branchial remnants and the associated colorectal hypoganglionosis based on radiological studies. The patient refused any further operative interventions. Therefore, the option of conservative treatment of hypoganglionosis with holobiotics consisting of prebiotics, probiotics and postbiotics, laxatives, dietary changes, lifestyle modifications, and dietary supplements started. All antibiotics were stopped. These therapies resulted in the resolution of residual first branchial remnants and recurrent MRSA infections with the improvement in the facial nerve palsy from grade V to grade III-IV together with an excellent cosmetic and functional result. The patient is doing well at follow-ups being infection-free for 18 months and repeat contrast-enhanced computed tomogram (CECT) has shown complete resolution of the residual cyst, sinus, and fistula with fibrosis.
Congenital anomalies of the branchial apparatus involving the second branchial one are the most common. The first branchial anomalies are very rare, with an incidence of less than 8% of all branchial anomalies [1] They are typically misdiagnosed and inappropriately managed for several years before being correctly diagnosed and appropriately treated [2]. The delay in diagnosis can result in unnecessary investigations, iatrogenic injuries, unnecessary burdens, and stress for the patient [3-5]. We present a unique case of type II left first branchial cyst, sinus, and fistula in association with bilateral second branchial fistulas and hypoganglionosis presenting as an acute abscess simulating nonspecific abscess and resulting in injury to the facial nerve and recurrent MRSA infections in the residual cyst and sinus. In addition, we describe the novel technique of successful conservative treatment of hypoganglionosis to help resolve these problems incidentally as sclerotherapy was impossible and the patient was afraid of operation.
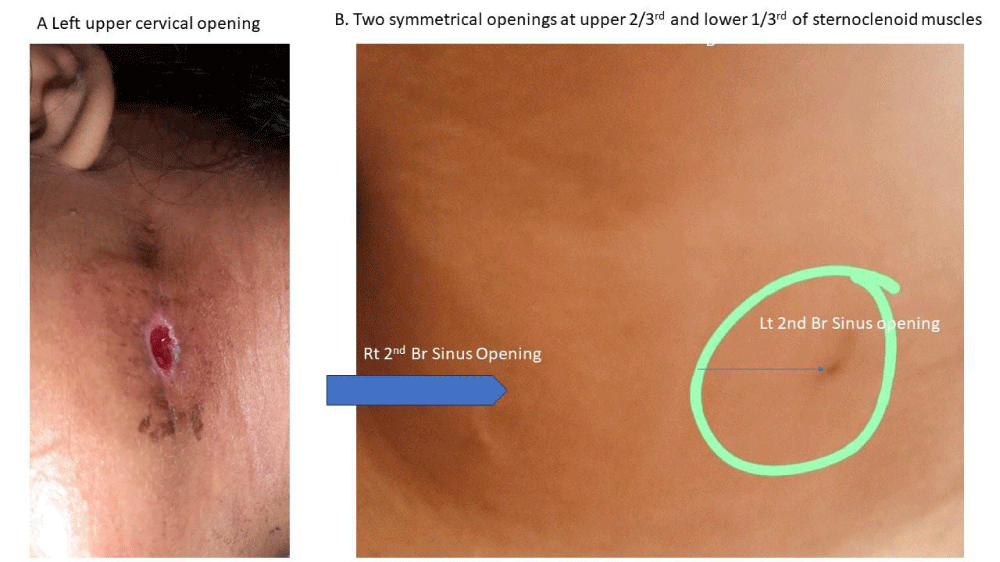
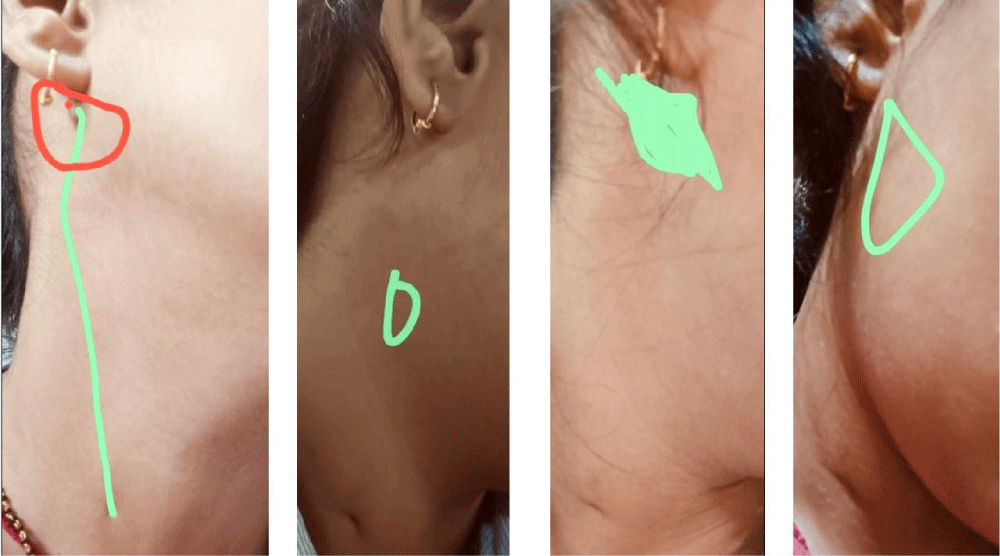
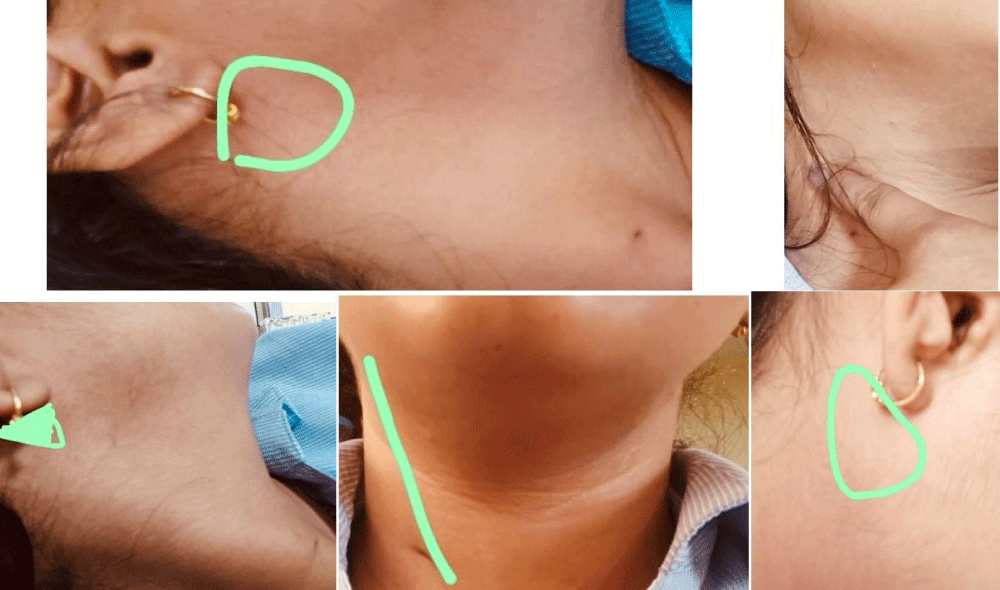
A 24-year-old female with normal-term vaginal delivery following uneventful pregnancy was noted to have three openings in the neck at birth- one at the left upper cervical areas near the angle of the mandible (Figure 1A) and two symmetrical openings in the lower part of the anterior left neck discharging glary fluid intermittently (Figure 1B). Patient had a background of chronic abdominal gaseous distention, recurrent bloating, central and left lower quadrant intermittent pain and chronic constipation since early infancy but otherwise was apparently healthy.
Figure 1: Clinical photographs. A left first branchial cyst and sinus B. bilateral second branchial sinuses.
On 5th July 2020, during the COVID infection 1st wave peak period, suddenly the cloudy white creamy discharge that was coming out from the left upper cervical sinus stopped. The patient developed acute diffuse painful swelling around the left upper cervical region opening associated with the hot, red, and tender mass lesion (Figure 2A). Patient presented to a private Head and Neck/ENT surgeon. Laboratory studies showed high inflammatory markers, COVID-19 tests were negative, and a provisional diagnosis of acute suppurative lymphadenitis was made and triple antibiotics were given for 15 days without any success. The patient underwent incision and drainage. Following drainage of the pus, the healing wound showed a recurrence of the discharging sinus again (Figure 2B).
Figure 2: First operation A. immediate post-operative and B. post-operative recurrent sinus.
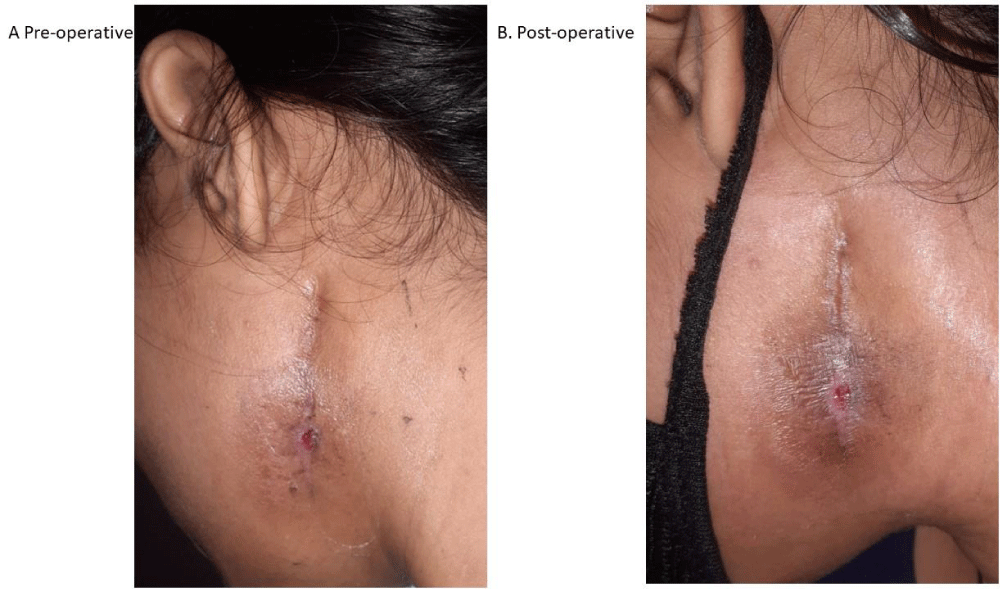
On 24th August 2020, a sinogram through the recurrent sinus observed a small 1.8-2 cms long sinus tract in the left submandibular location with posterosuperior or peripheral extension of the sinus tract without any branching (Figure 3A,B.) The surgeon decided to go ahead with formal exploration and total excision of the remaining sinus and the cyst.
Figure 3: Sinogram A. Filling phase B. Complete sonogram.
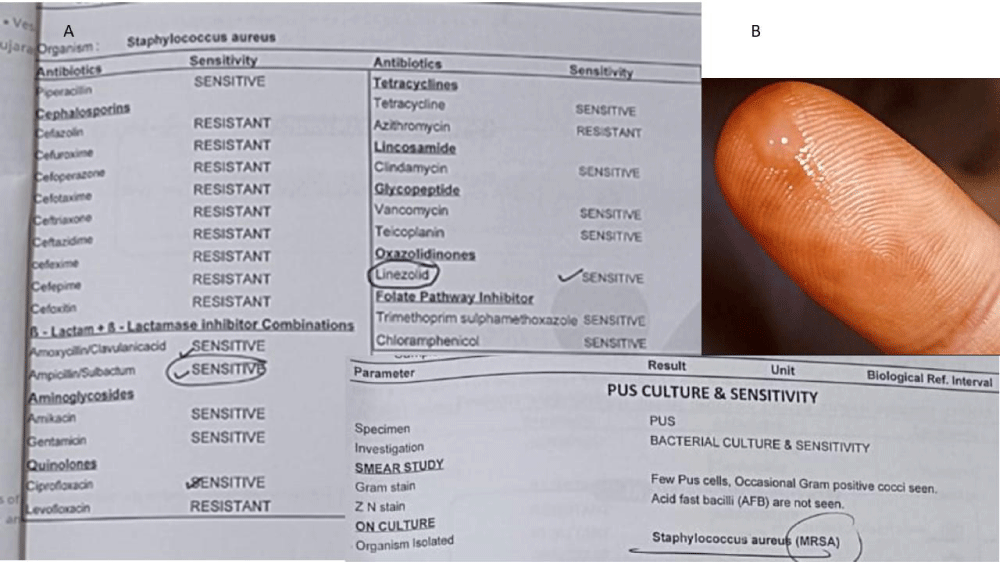
On 4th September 2020, the excision was attempted by extending the initial small central incision superiorly behind the external ear but not making it Y incision in front of the ear as it was thought to be related to the submandibular salivary gland based on the sinogram report and inferiorly to allow wider access (Figure 4A,B). Nearly 3-4 cm of the sinus tract was removed. However, it resulted in facial nerve palsy grade V significantly affecting the quality of life with injury to the surrounding parotid gland.
Figure 4: Post-second operation A. Superior extension B. Inferior extension.
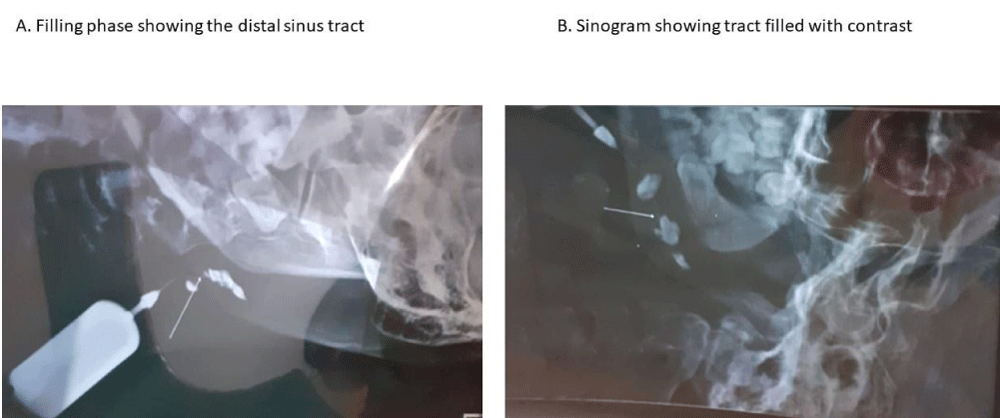
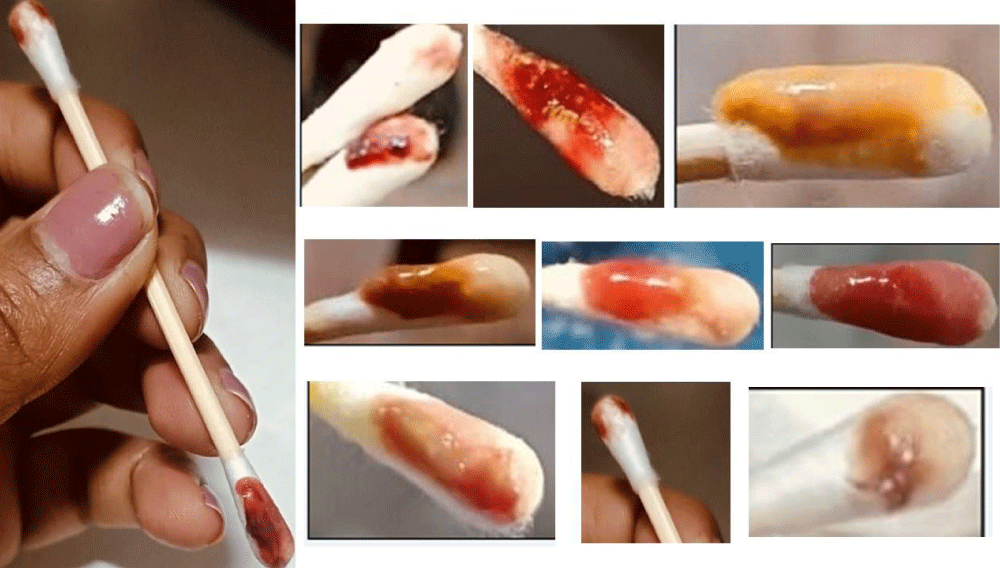
Post-operatively patient developed recurrent discharging sinus, residual cyst infections, and later on persistent infections. The patient started searching the literature globally and found few experts who have reported preservation of the facial nerve and parotid gland who suggested getting the pus microscopy, culture, and sensitivity studies which showed MRSA Staphylococci aureus sensitive to linezolid and sulbactam plus requiring several intravenous broad-spectrum antibiotics (Figure 5A,B). A variety of discharges growing MRSA and having cholesterol crystals were observed and have been treated with a variety of oral and intravenous broad-spectrum antibiotics (Figure 6). On 23rd Nov 2021 an ultrasound showed a 12X9 mm isohypoechoic lesion noted in the superficial lobe of the left parotid glands having intraparotid lymphadenopathy.
Figure 5: A. MCS of the swabs from the discharge B. Typical cholesterol crystals in the discharge.
Figure 6: Variety of color and consistency of swabs from left first branchial cyst and sinus.
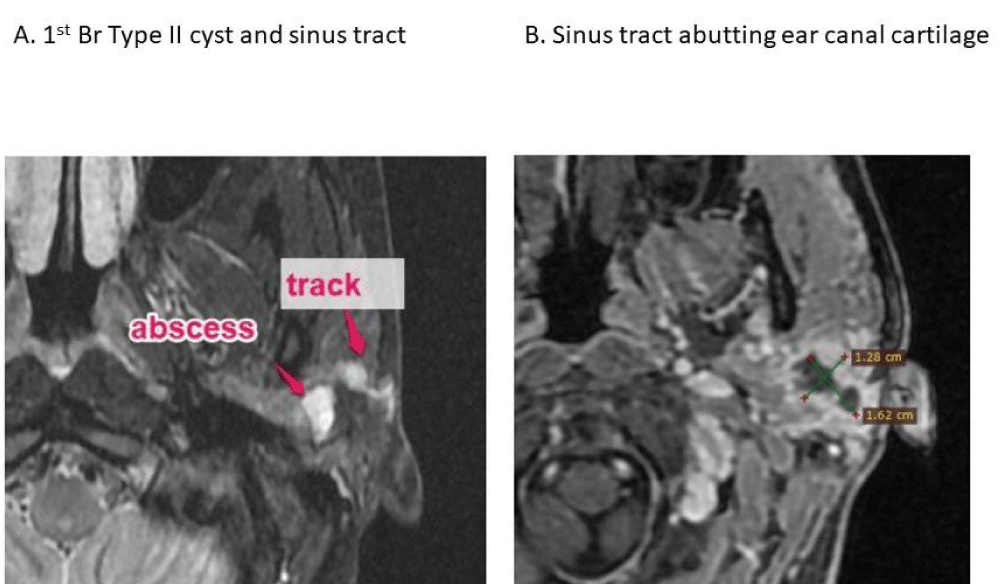
Magnetic resonance imaging (MRI) of the neck and parotid region was performed with high-resolution T1, T2, and STIR-weighted sections obtained in the sagittal, coronal, and axial planes. It showed loculated peripherally enhancing irregular wall fluid intensity area measuring 16 x 11 x 20 mm having a volume of 1.5-2.5CC involving the left parotid gland with diffuse enhancing edematous changes suggesting the possibility of parotitis with intraparotid abscess formation (Figure 7A). There was no evidence of extension of the lesion in the deep lobe parotid gland. T2 hypointense linear areas were noted in the superficial lobe of the parotid gland and surrounding the lesion possibility of fibrotic changes from previous surgery. A thin fluid-intensity tract was noted extending from the collection passing through the superficial parotid lobe laterally and extending up to the preauricular soft tissue just anterior and inferior to the external auditory canal terminating in subcutaneous tissue just outside the capsule of the posteroinferior surface of the parotid gland without obvious skin opening suggested impending sinus tract formation (Figure 7B). Approximate length of the sinus tract measured 1.5-1.8 cm. Another suspicious very short tract was noted posteroinferior to the external auditory canal terminating in deep subcutaneous tissue just outside the capsule of the superficial lobe of the parotid gland. Multiple mildly enlarged lymph nodes were noted in the left parotid region, within the left parotid gland, bilateral upper jugular region measuring 8 x 8 mm in the left parotid gland and 17 x 10 mm in the left upper jugular region.
Figure 7: MRI scan postoperatively showing A. residual cyst and B. sinus.
The patient started having fullness, tightness, and discomfort along the right 2nd brachial sinus near its tonsillar part of the tract especially during episodes of throat infection and upper respiratory tract infections while swallowing, etc. A subsequent ultrasound scan to see the status of the left infected branchial cyst and both 2nd branchial anomalies was carried out after a few antibiotic courses. The ill-defined heterogeneously hypoechoic area was noted in the superficial surface of the left parotid gland measuring 10 x 10 mm suggesting sequelae of residual chronic cavity. As compared to the previous study the size of the cavity was almost static with no obvious visualisation of the hypoechoic tract could be seen. Another sinus tract was noted with its external opening along the anterior surface of the sternocleidomastoid muscle the junction of mid and lower third. The tract was extending superiorly within the carotid space. However, it cannot be traced further superiorly above the level of hyoid suggestive of the possible tonsillar fossa communication with the possibility of a second branchial cleft fistula/sinus. Multiple enlarged lymph nodes were noted bilateral upper jugular and submandibular region. The largest measured 3 x 1 x 0.4 cm in right level II.
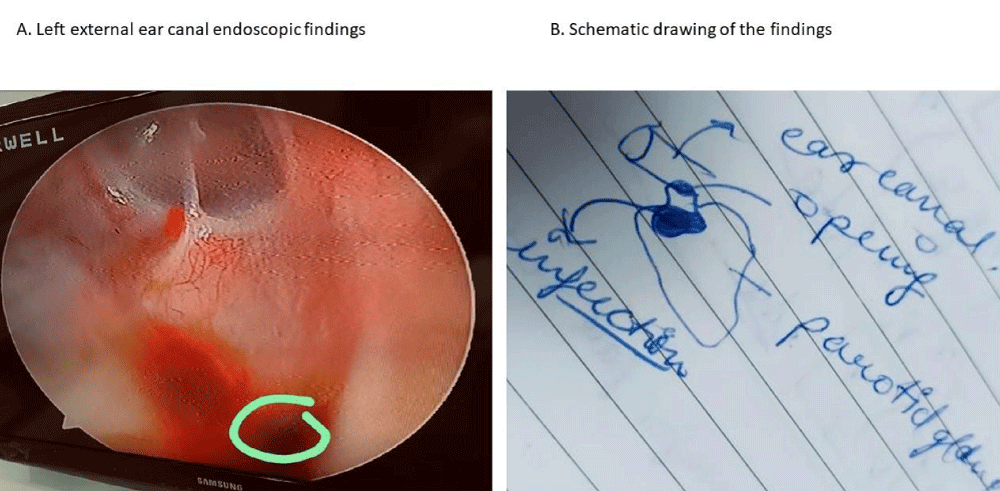
The ultrasound and magnetic resonance imaging showed a residual infected cyst and sinus opening in the left ear canal clinically as discharge. A diagnosis of branchial cyst type II of the first brachial cleft, cyst, and sinus/fistula was established with bilateral branchial fistulas of the second brachial remnants associated with hypoganglionosis based on radiological studies. Endoscopic examination confirmed the opening deep in the external ear canal at right angles to the canal and attempts at cannulation and sclerotherapy failed (Figure 8A,B).
Figure 8: A. Endoscopic findings and B. Schematic representation.
The patient had subsequent right upper second branchial fistula having poor drainage and recurrent infections (Figure 9). However, this started resolving once the conservative treatment of the associated congenital colorectal motility disorder of hypoganglionosis was started (Figure 10).
Figure 9: Inadequate drainage and repeated infections of right upper second brachial fistula before conservative treatment.
Figure 10: Post conservative treatment right upper second branchial fistula drainage and no infections.
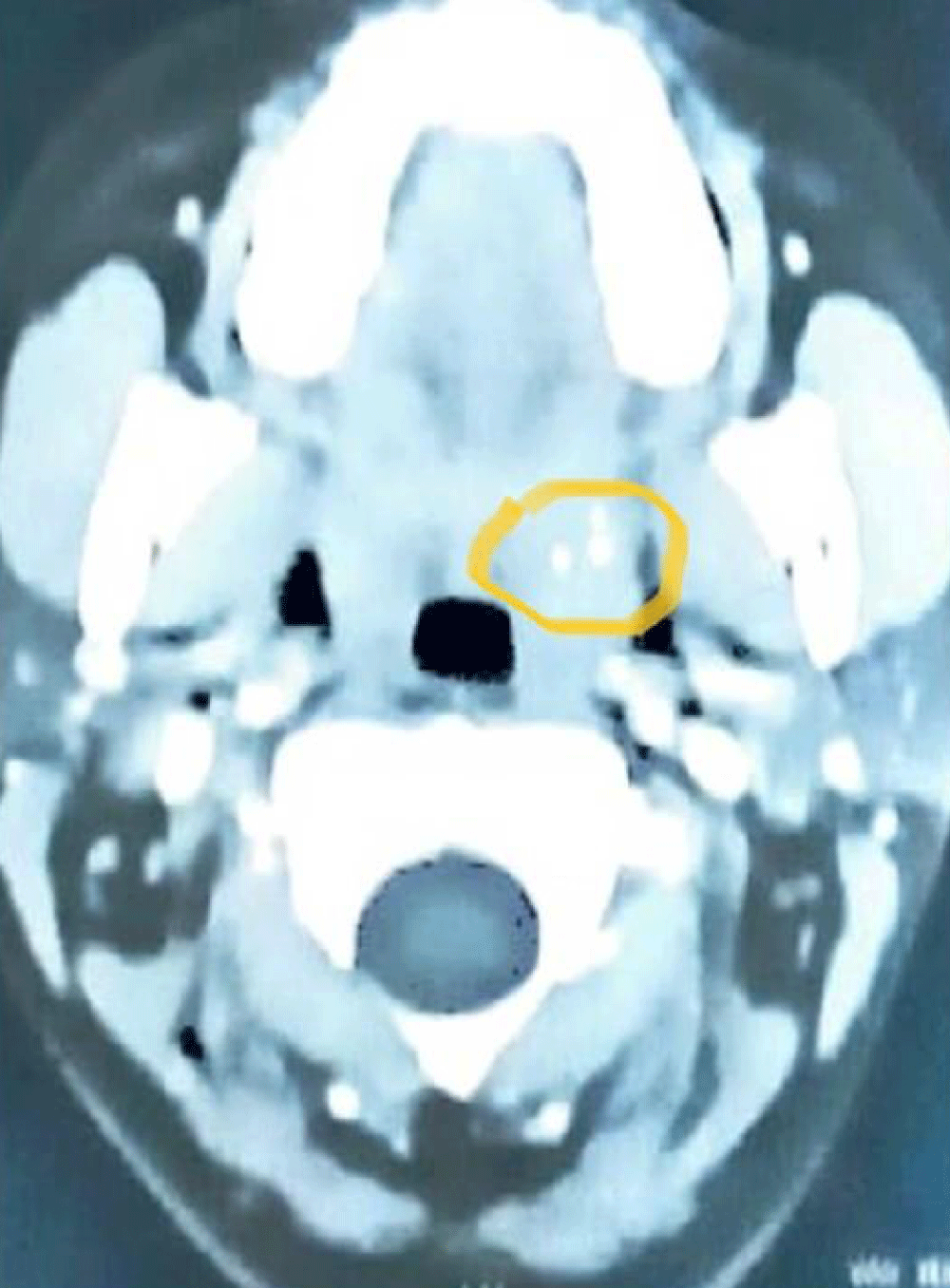
The plan of surgical exploration, excision of the residual cyst and sinus with preservation of the facial nerve and the parotid gland was explained to the patient but due to very traumatic and severe setback following facial nerve injury and several infections requiring multiple admissions and injections, the patient was scared to undergo any further open surgery in this area. The patient was treated conservatively stopping all antibiotics with oral hygiene and changing oral and gut microbiome. The patient has been infection and symptom-free for 18 months and repeat microscopy, culture, and sensitivity are negative. The contrast-enhanced computed tomogram (CECT) has shown complete resolution of the residual cyst and sinus with fibrosis (Figure 11). Following conservative management of the hypoganglionosis with holobiotics consisting of prebiotics, probiotics and postbiotics, laxatives, dietary changes, lifestyle modifications, and dietary supplements, patient made spectacular recovery around 60% recovery in facial palsy from initial grade V to current Grade III to IV by physiotherapy, b1, b6 and b12 neurovitamin supplementation and holobiotics, no pain, swelling or infections and excellent cosmetic and functional outcome.
Figure 11: Post-treatment CECT with resolution of infection and fibrosis only. Note an incidental tonsilolith on the left side highlighted with the circle.
Branchial congenital anomalies can present with a variety of presentations, with a cyst, sinus, fistula, or midline cervical cleft, and may first present with any one of the complications often making it difficult to make diagnosis at first sight [5]. The most common lesion is second branchial anomalies which were present bilaterally and proper detailed history and clinical examination would have alerted the clinician to the possible diagnosis in our case. A high index of suspicion should lead to at least simple investigations like an ultrasound scan to help see the complex underlying anatomy more easily comprehended. It is our practice to send all material for microscopy, culture, and sensitivity and all tissues for histopathology to give accurate post-operative diagnosis which was missed in our case but the post-operative infective complications and further investigations revealed the underlying pathology very clearly at a later stage.
Our team and institution have a deep interest in the head and neck congenital lesions in general and that of branchial apparatus in particular and the implications of the associated hypoganglionosis while shedding light on the intricacies of its manifestation in our specific patient case. Our team has done experimental fetal surgery in fetal rabbits and its extrapolation to translational, investigative, and therapeutic aspects of associated congenital colorectal secretomotility disorders [6-12].
The simultaneous presence of bilateral second branchial arch anomalies along with bilateral first arch anomalies is extremely rare, with only four such cases reported in the literature [13]. Branchial cleft anomalies are congenital aberrations of the first to fourth pharyngeal pouches. First branchial cleft anomalies are classified into 2 subtypes according to anatomical and histological features. Their diagnosis can be difficult and depends on radiological and histological findings. In contrast, the required treatment is surgical removal, owing to the high risk of infection or malignancy [14]. First branchial cleft anomalies are rare congenital malformations of the head and neck. They occur above the level of the hyoid bone and have a close anatomical relationship to the facial nerve owing to their embryologic origin [15].
Congenital first branchial cleft anomalies (FBCAs) in children often present with repeated swelling and purulence in Pochet’s triangle. Computed Tomogram, Ultrasound, and auricular endoscopy can assist in diagnosis and planning the surgical strategy. Complete excision in the non-infection stage as soon as possible is the first choice for the treatment [16]. Branchial cleft anomalies present in one of three forms: cysts, sinuses, or fistulae [17]. Awareness and consideration of the FBCA by ENT surgeons is key to preventing multiple invasive and futile operations [18]. FBCAs within the parotid gland involve more difficult and extensive appropriately aggressive surgical resection and the potential for morbidity related to facial nerve dissection [19].
FBCAs are often misdiagnosed for other cystic lesions occurring in the parotid gland and inadequately treated (incision and drainage or incomplete excision) leading to multiple recurrences [20]. Surgical complete excision is the gold standard and the approaches differ among the various types, careful preoperative planning, and protecting the facial nerve during resection of the tract are essential [21]. MRI findings were used to categorize FBCAs into three subtypes. FBCAs located between the subcutaneous tissue and parotid were classified as type IIa. FBCAs located between the deep and superficial lobes of the parotid were classified as type IIb. FBCAs located between the parotid and the carotid sheath were classified as type IIc [22]. Some type II FBCA patients had visible abnormalities lateral to the tympanic membrane. An otoscope was recommended for routine examination and combined during surgery to prevent recurrence [23]. Type II FBCAs had a close relationship with the facial nerve, especially when the lesion was located in the mandible angle [24]. Intraoperative microscope and facial nerve monitoring were necessary for protecting the facial nerve and decreasing the recurrent rate [25].
In a localised post-operative walled-off pathology, we prefer to do localised intervention rather than a major surgical undertaking as associated fibrosis and side pocket extensions can lead to more damage to the seventh nerve. The surgery needs to be reserved for the least invasive option and preservation of the facial nerve and parotid gland has many advantages [3-5]. The hypoganglionosis is a seen mainly in children and young adults (7-9). It has been reported in adults but it is rare to see in elderly patients (10). This can lead to chronic fecal retention leading to dysbiosis of the colon, intermittent or continuous ileocecal reflux, small bowel bacterial overgrowth with activation of the immune system network via Payer’s patches and causing malabsorption with multiple micronutrient deficiencies (11-12).
Our hypothesis is that in our case perhaps the association of the branchial anomalies with hypoganglionosis has been a risk factor in the predisposition of recurrent post-operative infective complications, especially after taking several courses of oral and parenteral broad-spectrum antibiotics serially by chronic alteration of the microbiome of the hindgut causing dysbiosis initially followed by midgut via ileocecal reflux and small bowel bacterial growth secondarily and tertiarily via feco-oral route altering oral and foregut microbiome which has been implicated in the development of gut and gut-derived recurrent infections in children, especially for those children who are not breastfed as per recommendations recently.
Congenital anomalies and their consequences on the branchial apparatus in general and the first branchial anomalies, in particular, are complex disorders with a wide range of gastrointestinal and extraintestinal-associated anomalies. Understanding the differential diagnosis of cervical masses and other conditions is crucial to targeted investigations, providing accurate diagnosis, and appropriate treatment to decrease perioperative complications. Evidence of associated second branchial sinus/fistula should alert the clinician to the possibility of first branchial congenital anomalies. The relationship between colorectal motility disorder and branchial apparatus anomalies needs to be explored. Traditional approaches of treating post-operative infective recurrent infective complications using broad-spectrum combined antibiotics need to be reviewed in view of increasing evidence of changing the microbiome with the help of diet, laxatives, supplements, and holo biotics which are safe, effective, non-invasive, and cheaper patient-friendly option.
Compliance with ethical standards
Funding: The authors are very grateful to Dr Dhaval R Govani MB BCh, MBA, Medical Director, PGICHR, and the associated University Teaching Hospitals, Rajkot for his personal interest and supervision for the ongoing gut secretomotility disorders and microbiome project and for providing much-needed financial support for the project through the Dhaval Govani Educational and Research Foundation Trust, Rajkot, Gujarat, India.
The authors are grateful to Dr. Jitendra J Govani, Family Physician, for prompt referral and long-term follow-up of this patient, Dr. Ramesh V Virani, Consultant Radiologist, for extensive imaging workup and reconstruction, and Dr. Rohan Ashit Chhaniara and Dr. Ashit P Chhaniara in providing help and support in the management of this case.
Ethics declarations
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from the patient.
- Li W, Zhao L, Xu H, Li X. First branchial cleft anomalies in children: Experience with 30 cases. Exp Ther Med. 2017 Jul;14(1):333-337. doi: 10.3892/etm.2017.4511. Epub 2017 May 24. PMID: 28672934; PMCID: PMC5488406.
- Adams A, Mankad K, Offiah C, Childs L. Branchial cleft anomalies: a pictorial review of embryological development and spectrum of imaging findings. Insights Imaging. 2016 Feb;7(1):69-76. doi: 10.1007/s13244-015-0454-5. Epub 2015 Dec 10. PMID: 26661849; PMCID: PMC4729717.
- Patel R, Kundra A, Judd O, Moir A, More B: Type II first branchial cyst and sinus excision with preservation of facial nerve and parotid gland. J Ped Surg Case Reports. 2013: 1: 1e4.
- King J, Patel R, Huddart SN. Congenital midline cervical cleft. Journal of Pediatric Surgery Case Reports. 2013; 1: 99-101.
- Narasimharao KL, Patel RV, Pathak IC. First branchial cleft sinus: a diagnostic trap for the unwary. Indian Pediatr. 1985 Jun;22(6):470-2. PMID: 3835147.
- Patel RV, Anthony FM, Govani ND, Govani DR, Panchasara N, Patel RR, Corracia R. Abdominal Wall Defects and Hernias-lessons learnt from observations from the experimental fetal surgery gastroschisis model in rabbits and their clinical extrapolation. Medp Pediatr Child Health Care. 2022; 1(1): mppchc-202201001, 2022, 1: 8-15.
- Govani DJ, Trambadia, RA, Chhaniara RA, Mirani ZR, Chhaniara AP, Midha PK, Swamy KB, Patel RV. Pre-Operative Diagnosis of Infantile Triad of Waugh’s Syndrome Associated with-Hypoganglionosis-Key Radiological Findings. Health Child Pediatr SMP. 2023; 1: 1-9.
- Govani DJ, Govani ND, Govani DR, Panchasara NG, Patel RR, Midha PK, Correia RC, Patel RV. Successful Conservative Management of Triple Pelvic Outlet Functional Obstruction Syndrome with Voiding, Menstrual and Bowel Dysfunctions in an Adolescent Girl with long term follow up. J Urol Neph St. 2023; 4(2): 425-31. JUNS.MS.ID.000181. DOI: 10.32474/JUNS.2023.04.000181
- Govani DJ, Govani ND, Govani DR, Panchasara NG, Patel RR, Midha PK, Correia RC, Patel RI. Successful Conservative Management of Dysfunctional Elimination Syndrome Associated with Micronutrient Deficiencies, Recurrent Juvenile Allergic Urethritis and Penoscrotal Edema. Med Discoveries. 2023; 2(1): 1018.
- Detroja PL, Trambadia RA, Chhaniara RA, Mirani ZR, Midha PK, Patel RV. Mini-series of variety of giant renal calculi as sociated with pelviureteric junction obstruction and hypoganglionosis. Open J Clin Med Images. 2023; 3(1): 1095.
- Zaparackaite I, Singh SJ, Bhattacharya D, Kansagra PJ, Swamy KB, Correia RC, Midha PK, Patel RV. Exploring the characteristics of gut microbiome in patients of Southern Fujian with hypocitraturia urolithiasis and constructing clinical diagnostic models. Int Urol Nephrol. 55: 1917–1929. by Wang, et al. Int Urol Nephrol 55-Manuscript - UROL-D-23-01558.
- Govani DJ, Trambadia RA, Chhaniara RA, Mirani ZR, Midha PK, Correia RC, Patel RV. "Is anemia frequently recognized in gastroschisis compared to omphalocele? A multicenter retrospective study in southern Japan" by Sugita, K et al. Pediatr Surg Int. 2022 Dec 1;39(1):26. doi: 10.1007/s00383-022-05288-8. PMID: 36454276.
- Shah S, Prabhat D, Bodhanwala M. Coexistence of Bilateral First and Second Branchial Cleft Anomalies: A Rare Case Report. Indian J Otolaryngol Head Neck Surg. 2022 Oct;74(Suppl 2):2252-2255. doi: 10.1007/s12070-020-02115-1. Epub 2020 Sep 2. PMID: 36452581; PMCID: PMC9702133.
- Milani A, Magliulo G, Rossetti V, Polimeni R, Pace A. Isolated First Branchial Cleft Anomalies of the External Auditory Canal. Am J Case Rep. 2022 Nov 7;23:e936809. doi: 10.12659/AJCR.936809. PMID: 36342864; PMCID: PMC9650556.
- Olivas AD, Sherman JM. First Branchial Cleft Anomalies. Op Tech in Otolaryngology-Head and Neck Surgery. 2017; 28(3): 151-55. DOI: https://doi.org/10.1016/j.otot.2017.05.012
- Chen W, Xu M, Wang Q, Xu R, Chen J, Xu H, Li X. Congenital first branchial cleft anomalies in children: a study of 100 surgical cases and a review of the literature. Eur Arch Otorhinolaryngol. 2023 Jan;280(1):425-433. doi: 10.1007/s00405-022-07607-0. Epub 2022 Aug 30. PMID: 36040517.
- Coste AH, Lofgren DH, Shermetaro C. Branchial Cleft Cyst. 2023 Jun 30. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 29763089.
- Ash J, Sanders OH, Abed T, Philpott J. First Branchial Cleft Anomalies: Awareness Is Key. Cureus. 2021 Dec 24;13(12):e20655. doi: 10.7759/cureus.20655. PMID: 34976546; PMCID: PMC8712219.
- Wilson J 4th, Jaju A, Wadhwani N, Gorelik M, Johnston D, Rastatter J, Bhushan B, Hazkani I, Fudyma I, Maddalozzo J. Reworking Classification of First Branchial Cleft Anomalies. Laryngoscope. 2023 Jun 5. doi: 10.1002/lary.30783. Epub ahead of print. PMID: 37272866.
- Kumar R, Sikka K, Sagar P, Kakkar A, Thakar A. First branchial cleft anomalies: avoiding the misdiagnosis. Indian J Otolaryngol Head Neck Surg. 2013 Jul;65(3):260-3. doi: 10.1007/s12070-013-0641-y. Epub 2013 Mar 19. PMID: 24427578; PMCID: PMC3696159.
- Li W, Zhao L, Xu H, Li X. First branchial cleft anomalies in children: Experience with 30 cases. Exp Ther Med. 2017 Jul;14(1):333-337. doi: 10.3892/etm.2017.4511. Epub 2017 May 24. PMID: 28672934; PMCID: PMC5488406.
- Liu W, Chen M, Liu B, Zhang J, Ni X. Clinical Analysis of Type II First Branchial Cleft Anomalies in Children. Laryngoscope. 2021 Apr;131(4):916-920. doi: 10.1002/lary.29049. Epub 2020 Aug 26. PMID: 32846011.
- Liu W, Chen M, Yang Y, Shao J, Ni X, Zhang J. The Treatment for Type II First Branchial Cleft Anomalies With Abnormalities Lateral to the Tympanic Membrane. Ear Nose Throat J. 2022 Dec 21:1455613221147344. doi: 10.1177/01455613221147344. Epub ahead of print. PMID: 36542778.
- Liu W, Liu B, Chen M, Hao J, Yang Y, Zhang J. Clinical analysis of first branchial cleft anomalies in children. Pediatr Investig. 2018 Oct 17;2(3):149-153. doi: 10.1002/ped4.12051. PMID: 32851251; PMCID: PMC7331312.
- Liu W, Chen M, Hao J, Yang Y, Zhang J, Ni X. The treatment for the first branchial cleft anomalies in children. Eur Arch Otorhinolaryngol. 2017 Sep;274(9):3465-3470. doi: 10.1007/s00405-017-4648-y. Epub 2017 Jun 20. PMID: 28634783.