More Information
Submitted: July 01, 2023 | Approved: July 12, 2023 | Published: July 13, 2023
How to cite this article: Huyen PX, Nhan HH, The PT, Hoa CC. Transcanal Endoscopic Excision of Glomus Tympanicum in can tho Ent Hospital: Three Cases Report. Heighpubs Otolaryngol Rhinol. 2023; 7: 001-004.
DOI: 10.29328/journal.hor.1001026
Copyright License: © 2023 Huyen PX, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: 188Re-liposome; HNSCC; Cerenkov luminescent imaging; microRNA expressive profile; prognostic factors
Transcanal Endoscopic Excision of Glomus Tympanicum in can tho Ent Hospital: Three Cases Report
Pham Xuan Huyen, Ho Le Hoai Nhan, Pham Thanh The and Chau Chieu Hoa*
Can Tho Ear Nose Throat Hospital, Can Tho 900000, Vietnam
*Address for Correspondence: Chau Chieu Hoa, Can Tho Ear Nose Throat Hospital, Can Tho 900000, Vietnam, Email: [email protected]
Glomus tympanicum (GT) is a highly vascular, benign, and slow-growing tumor of the middle ear. It can be confused with other common ear diseases such as acute middle ear infection, otitis media with effusion, ear trauma… It is accurately diagnosed by history and endoscopy. CT scan showing: the presence of eroding jugular bulb is the most important thing to distinguish glomus tympanicum and glomus jugulare and assess the extension of the tumor to make good surgical planning. We present here the three cases in Can Tho ENT hospital: where total excisions were achieved trans-canal endoscopically without embolization. These procedures were safe, quick, and effective due to the better visualization of the surgical field with the endoscope.
Glomus tumors, also known as non-chromaffin cell paraganglioma, arise from the neural crest cells [1]. They are rare tumors, representing less than 0.5% of all head and neck tumors [2]. Glomus tumors are classified into types depending on where they begin to grow: tympanicum, jugulare, glomus vagale, or carotid body. In this article, we just discuss glomus tympanicum [2-4]. It is a highly vascular, benign, and locally invasive tumor of the middle ear usually originating along the tympanic (Jacobson’s) or auricular (Arnold’s) nerve. It is the most common primary neoplasm of the middle ear and the second most common tumor of the temporal bone [1,5,6].
From 2021 to 2022, there were three cases of glomus tympanicum tumors operated by trans-canal endoscopic excision in Can Tho ENT hospital. All of the cases are female and aged from 44 to 60 years old.
- Clinical diagnosis: complaining unilateral pulsatile tinnitus, reduced hearing, aural fullness, and recurrent ear bleeding [7-9].
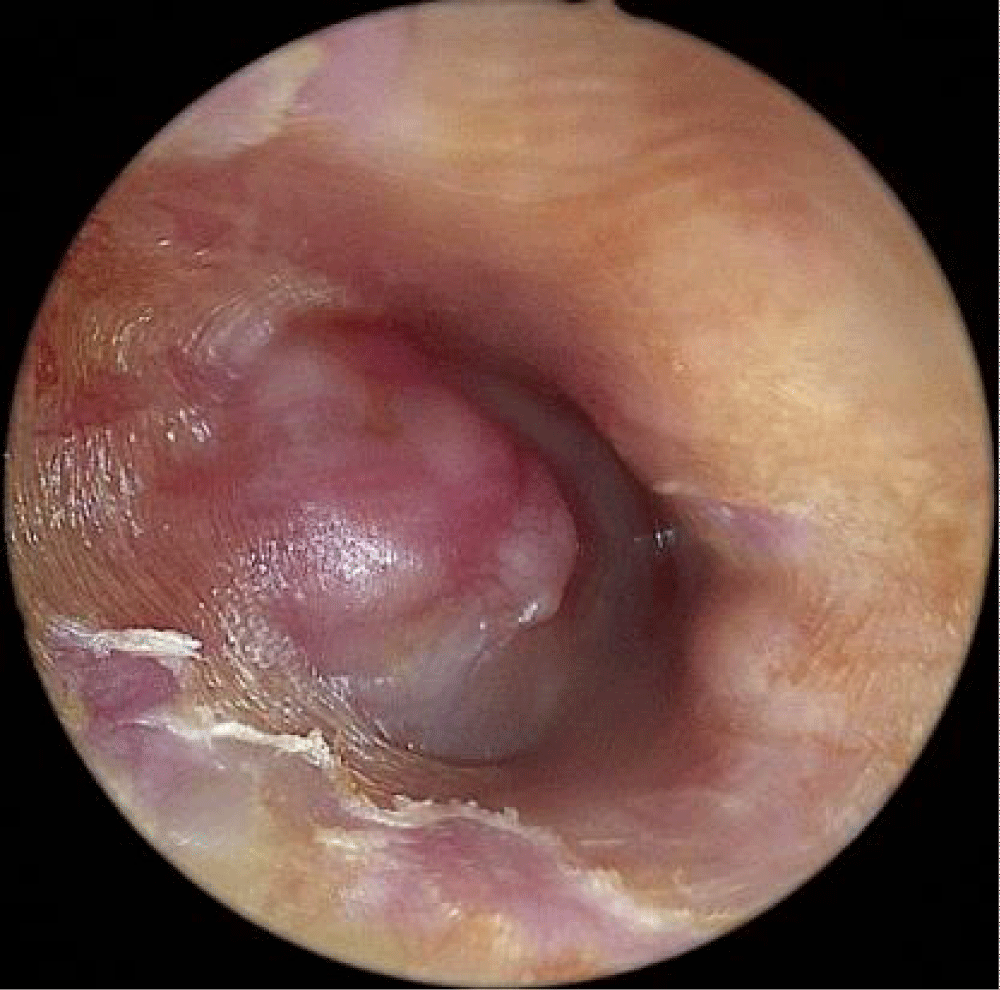
- Endoscopic examination: showed a red pulsatile mass behind an intact tympanic membrane [1,10].
- Hearing test: showed moderate mixed hearing loss.
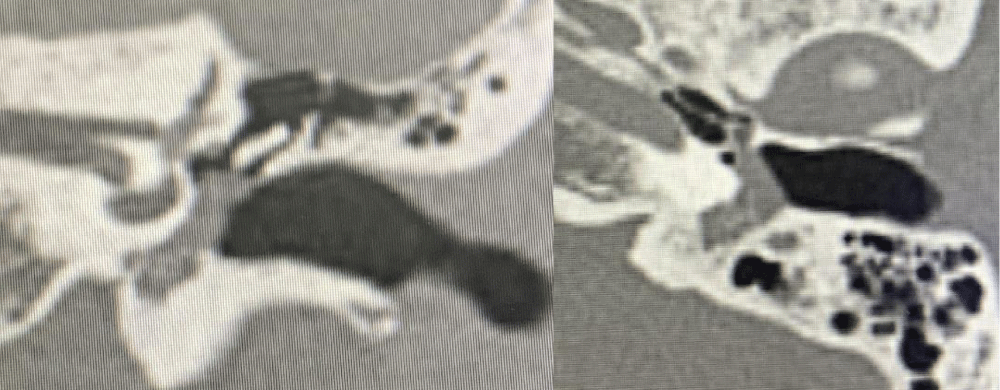
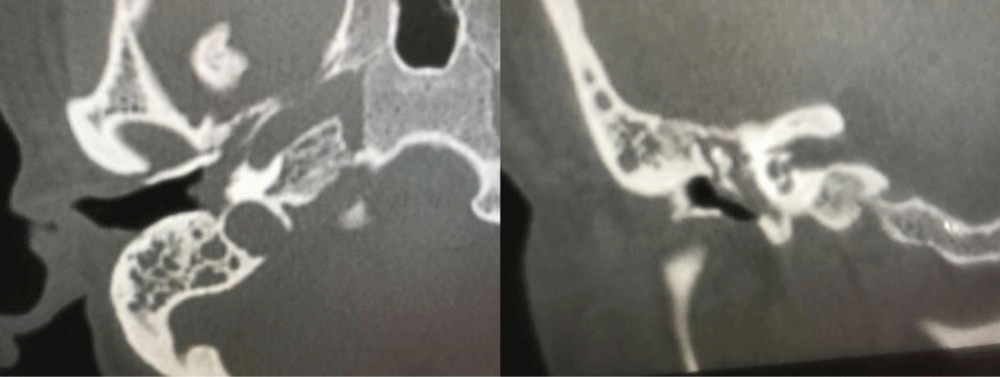
- CT scan showed the presence of a mass in the mesotympanum, epitympanum, hypotympanum, and no eroding jugular bulb [1,11,12].
- Histology: paragangliomas with polyhedral shape [2].
- Grade Definition (Glasscock- Jackson Classification) [1,2]:
1. Tumor margins are completely visible on otoscopy
2. Tumor fills the middle ear
3. Tumor fills the middle ear and the mastoid
4. The tumor extends through the tympanic membrane and into the external ear canal.
Classification of the tumor helps make a good plan and choose the proper surgical approach by trans-canal endoscopy or microscopy.
Case 1
A 44-year-old female patient presented to us with a history of pulsatile tinnitus, aural fullness, and progressive right-sided hearing loss over 7 months. She was treated in some clinics but no relief. There was no history of ear discharge, ear pain, or any other symptoms Figures 1-3.
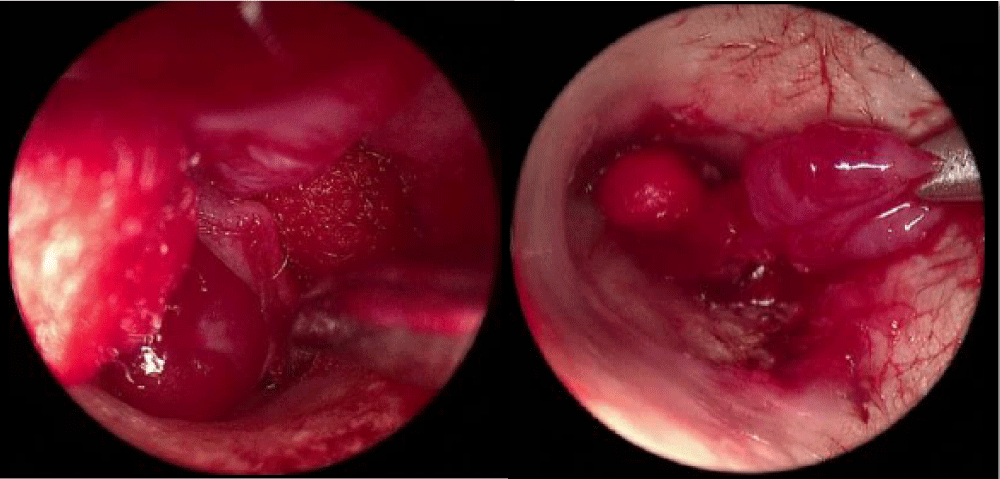
Figure 1: A red pulsatile mass was observed under the entire of the tympanic membrane.
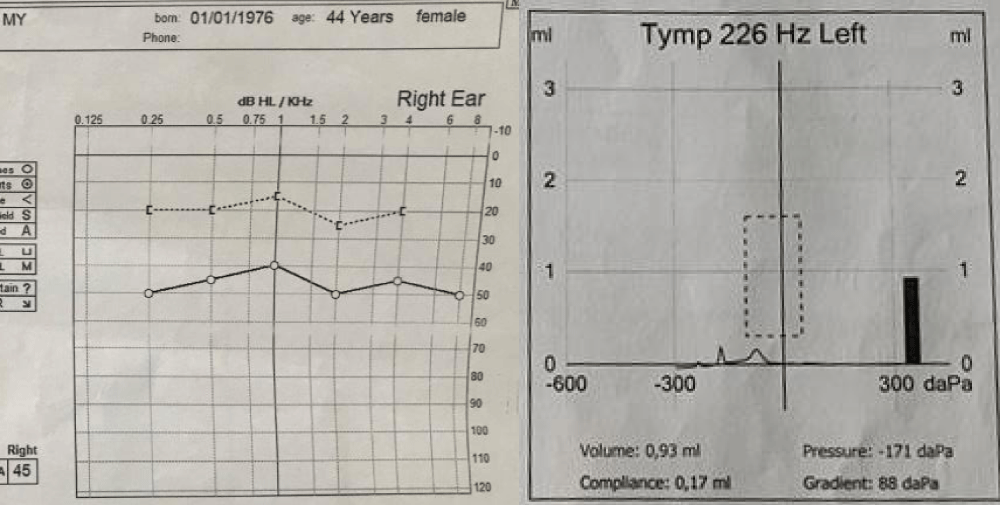
Figure 2: Audiogram with moderate mixed hearing loss 45dB and tympanometry had a sine graph shape
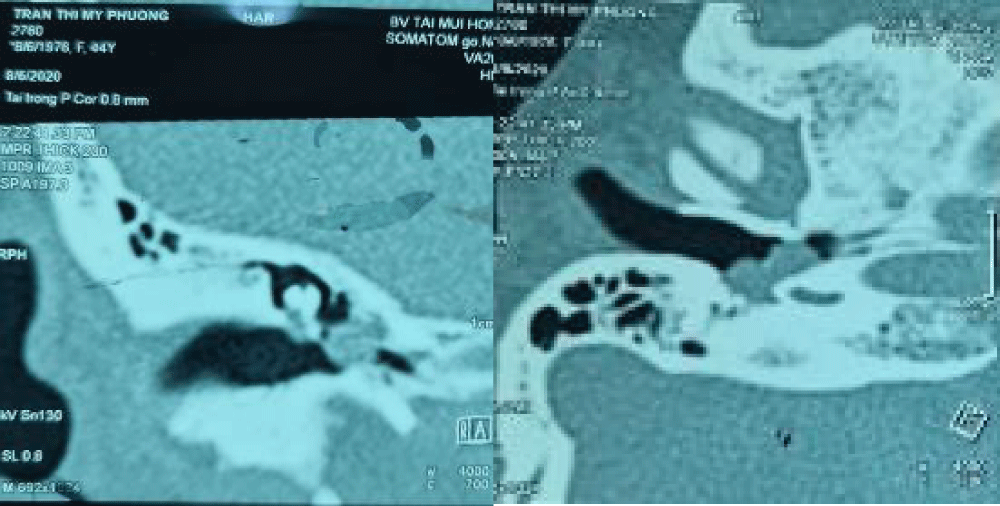
Figure 3: A tumor in the tympanic cavity and hypotympanum, not spread to the mastoid and does not erode the jugular bulb.
- Diagnosis: glomus tympanicum type II.
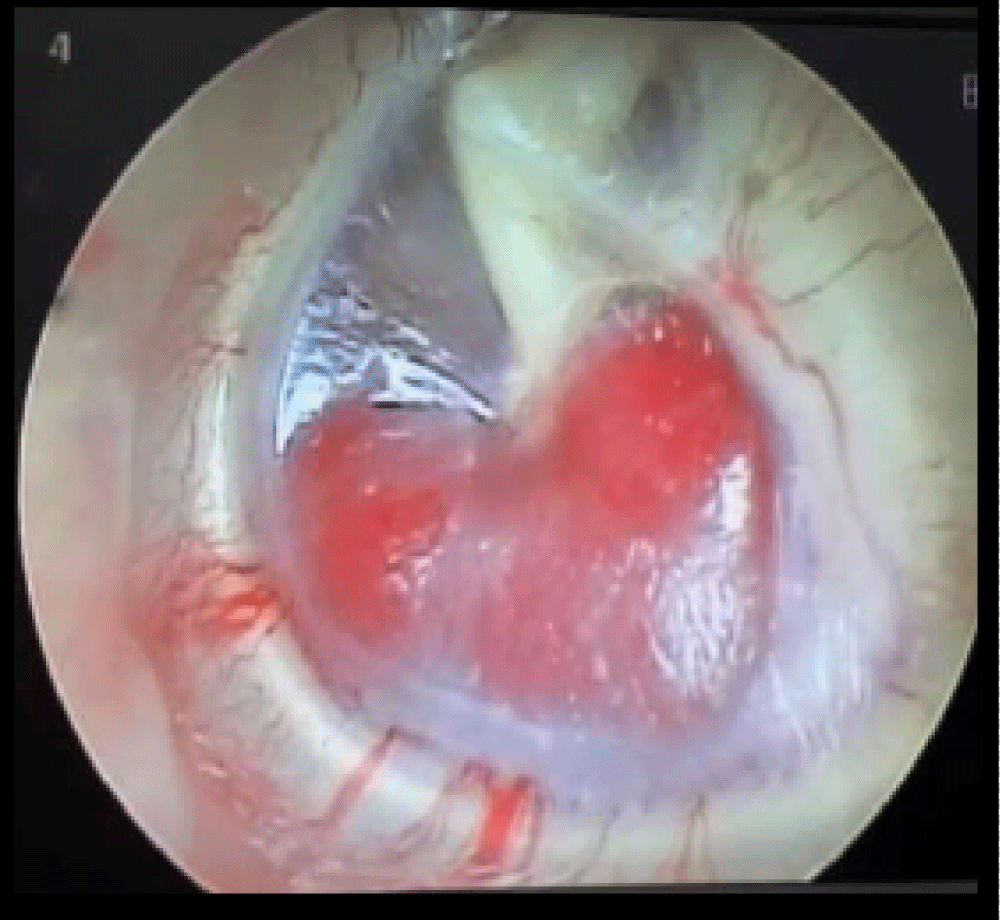
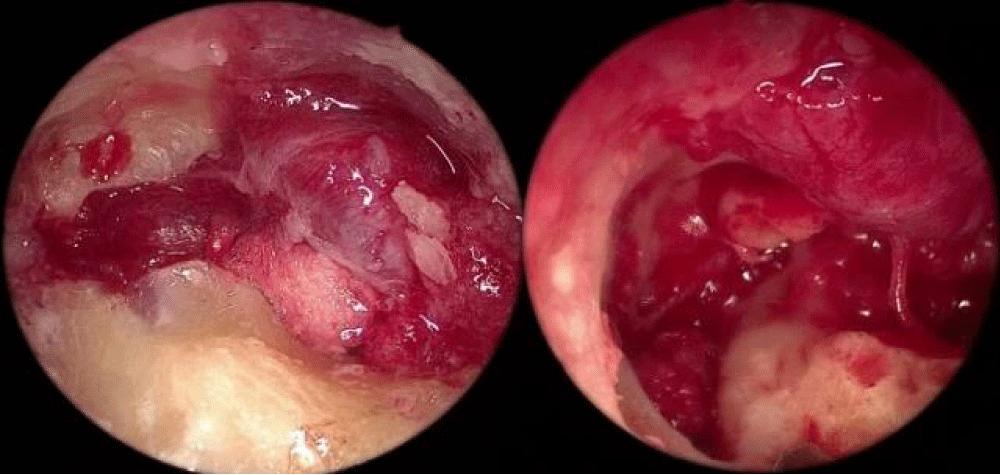
- Procedure: we started with a trans-canal endoscopic approach with a 00 scope. After adrenaline was injected and the tympanomeatal flap was elevated using a round knife, the pulsatile mass immediately came into view. The tumor filled the mesotympanum and hypotympanum with its base originating from a vessel at the promontory. It was completely removed with forceps which led to bleeding, and controlled by compressing with an adrenaline cotton ball. The tumor was successfully removed completely in two hours. After surgery, the patients have no more pulsatile tinnitus and their hearing level were improved Figure 4.
Figure 4: Endoscopic view of tumor removal of case 1.
Case 2
A 59-year-old female patient presented to us with a history of pulsatile tinnitus and progressive left-sided hearing loss for nearly 2 years Figures 5,6.
Figure 5: A red pulsatile mass was observed under the inferior half of the tympanic membrane.
Figure 6: Showing tumor in the tympanic cavity and spread to the hypotympanum close to the carotid artery but not eroding it.
- Hearing test: audiogram showed mild conductive hearing loss of 37dB and tympanometry had a sine graph shape.
- Diagnosis: glomus tympanicum type II.
- Procedure: similar to case 1 but we were more careful when assessing the tumor in the hypotympanum to prevent bleeding.
Case 3
A 46-year-old female patient presented to us with a history of pulsatile tinnitus, ear pain, progressive right-sided hearing loss, headache, and runny nose over 4 months. The patient was diagnosed with acute otitis media rhinosinusitis. After taking some assessments, she was diagnosed with glomus tympanicum Figures 7,8.
Figure 7: A pulsatile polypoidal vascular mass pushing right tympanic membrane.
Figure 8: A tumor in the tympanic cavity and hypotympanum, epitympanum, antrum and no eroded jugular bulb.
- Hearing test: audiogram showed average conductive hearing loss of 50dB and tympanometry had a sine graph shape.
- Diagnosis: glomus tympanicum type III.
- Procedure: The endoscopic trans-canal modified canal-wall-down mastoidectomy. We opened the attic by curetting the scutum and open the antrum by drilling the superior bony canal wall. After that drilled the canal wall down partially to exposure of the tumor clearly. The tumor filled the epitympanum, mesotympanum, and hypotympanum and surrounded the ossicular chain. We had to remove the incus to excise the whole tumor. After surgery, the hearing level decrease, and need to perform ossiculoplasty Figure 9.
Figure 9: Endoscopic view of tumor removal of case 3.
The surgical approach should be chosen according to the extension and the size of the glomus. We found that a total endoscopic excision can apply for Glasscock-Jackson type I, II, and type III with diploic or sclerotic mastoid. The development of this surgical technique provides better exposure and access, therefore leading to safe, quick, and effective tumor removal without sutures or canaloplasty.
- Manjunath HA, Sridurga J, Suresh Babu N. Glomus tympanicum type III – with delayed postoperative facial palsy: our experience. International J Otol. 2019.
- Offergeld C, Brase C, Yaremchuk S, Mader I, Rischke HC, Gläsker S, Schmid KW, Wiech T, Preuss SF, Suárez C, Kopeć T, Patocs A, Wohllk N, Malekpour M, Boedeker CC, Neumann HP. Head and neck paragangliomas: clinical and molecular genetic classification. Clinics (Sao Paulo). 2012;67 Suppl 1(Suppl 1):19-28. doi: 10.6061/clinics/2012(sup01)05. PMID: 22584701; PMCID: PMC3328838.
- Gulati K. Unusual presentation of a large glomus tympanicum with a coexisting cholesteatoma. Clin Case Rep. 2020 Jul 22;8(12):2429-2432. doi: 10.1002/ccr3.3175. PMID: 33363754; PMCID: PMC7752363.
- Baba Y. Glomus tympanicum paraganglioma. Radiopaedia.org. 2021.
- Leonardo Ordoñez- Ordoñez, Fabio Leon, Juanita Beltran. A case of glomus tympanicum during Stapedotomy Surgery for Otosclerosis. J Clin Case report. 2021; 4(4): 82-85.
- Lee SJ, Lee SY, An GS, Lee K, Choi BY, Koo JW, Song JJ. Treatment Outcomes of Patients with Glomus Tympanicum Tumors Presenting with Pulsatile Tinnitus. J Clin Med. 2021 May 27;10(11):2348. doi: 10.3390/jcm10112348. PMID: 34071897; PMCID: PMC8198089.
- Teh CS, Azrina A, Fadzilah I, Prepageran N. Transcanal endoscopic excision of glomus tympanicum: A case report. Med J Malaysia. 2020 Mar;75(2):189-190. PMID: 32281609.
- Kumar G, Andreou Z, Virk JS, Owa A. Unusual presentation of glomus tympanicum tumour: New bone formation in the middle ear. World J Clin Cases. 2014 Sep 16;2(9):463-5. doi: 10.12998/wjcc.v2.i9.463. PMID: 25232551; PMCID: PMC4163770.
- Priyanka M, Anjali L, Amit KT. Glomus tympanicum: clinical presentation, management, and outcomes. India Journal of Otology. 2021.
- Noel JE, Sajjadi H. KTP-laser-assisted endoscopic management of glomus tympanicum tumors: A case series. Ear Nose Throat J. 2018 Dec;97(12):399-402. doi: 10.1177/014556131809701209. PMID: 30540890.
- Daneshi A, Asghari A, Mohebbi S, Farhadi M, Farahani F, Mohseni M. Total Endoscopic Approach in Glomus Tympanicum Surgery. Iran J Otorhinolaryngol. 2017 Nov;29(95):305-311. PMID: 29383310; PMCID: PMC5785109.
- Ohki M, Kikuchi S. A Small Glomus Tympanicum Tumor Resected by Minimally Invasive Transcanal Endoscopic Approach. Case Rep Otolaryngol. 2019 Jul 9;2019:5780161. doi: 10.1155/2019/5780161. PMID: 31360569; PMCID: PMC6652060.
- Appannan VR, Md Daud MK. Glomus tympanicum. Malays Fam Physician. 2018 Apr 30;13(1):45-48. PMID: 29796211; PMCID: PMC5962235.
- Jackson CG, Glasscock ME 3rd, Harris PF. Glomus Tumors. Diagnosis, classification, and management of large lesions. Arch Otolaryngol. 1982 Jul;108(7):401-10. doi: 10.1001/archotol.1982.00790550005002. PMID: 6284098.
- Raza SS, Nadeem MD, Hussain AK , Saboor H. Glomus tympanicum: A case report. Khyber Medical College. Peshawar. 2017.