More Information
Submitted: December 10, 2022 | Approved: December 28, 2022 | Published: December 29, 2022
How to cite this article: Sai YRKM. Evolving Paradigms in Strep Throat: From Epidemiology to Advanced Therapeutics - A Comprehensive Overview. Heighpubs Otolaryngol Rhinol. 2022; 6: 001-010.
DOI: 10.29328/journal.hor.1001025
Copyright License: © 2022 WangSai YRKM. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Evolving Paradigms in Strep Throat: From Epidemiology to Advanced Therapeutics - A Comprehensive Overview
Sai YRKM*
GITAM Institute of Sciences, GITAM University, Visakhapatnam, Andra Pradesh, India
*Address for Correspondence: Sai YRKM, GITAM Institute of Sciences, GITAM University, Visakhapatnam, Andra Pradesh, India, Email: [email protected]
Strep throat, a common affliction known for its hallmark symptom of a severe and sudden sore throat, is caused by the bacterium Streptococcus pyogenes, classified under Group-A Streptococcus (GAS) [1]. This condition not only impacts millions globally but also carries the risk of severe complications if left untreated [2]. Understanding strep throat goes beyond recognizing its symptoms; it entails an appreciation of its transmission dynamics, potential complications, and the evolving landscape of treatment and prevention strategies [3].
The importance of delving deep into the understanding of strep throat cannot be overstated. Traditionally viewed through the lens of its clinical manifestations and treatment modalities, recent research has begun to uncover layers of complexity in its epidemiology, resistance patterns, and the long-term implications for those affected [4]. This article seeks to provide a nuanced exploration of strep throat, integrating traditional knowledge with the latest advancements in medical research to offer a comprehensive overview.
Recent nuances in the understanding of strep throat involve a multidimensional approach, considering factors such as genetic predispositions, environmental influences, and the intricate interplay between the host immune system and bacterial virulence factors [5]. Studies have shown that certain genetic markers may predispose individuals to more severe forms of the disease or increase their susceptibility to complications such as rheumatic fever, a serious condition that can follow untreated strep throat [6]. This has significant implications for personalized medicine and the potential for targeted interventions in high-risk populations.
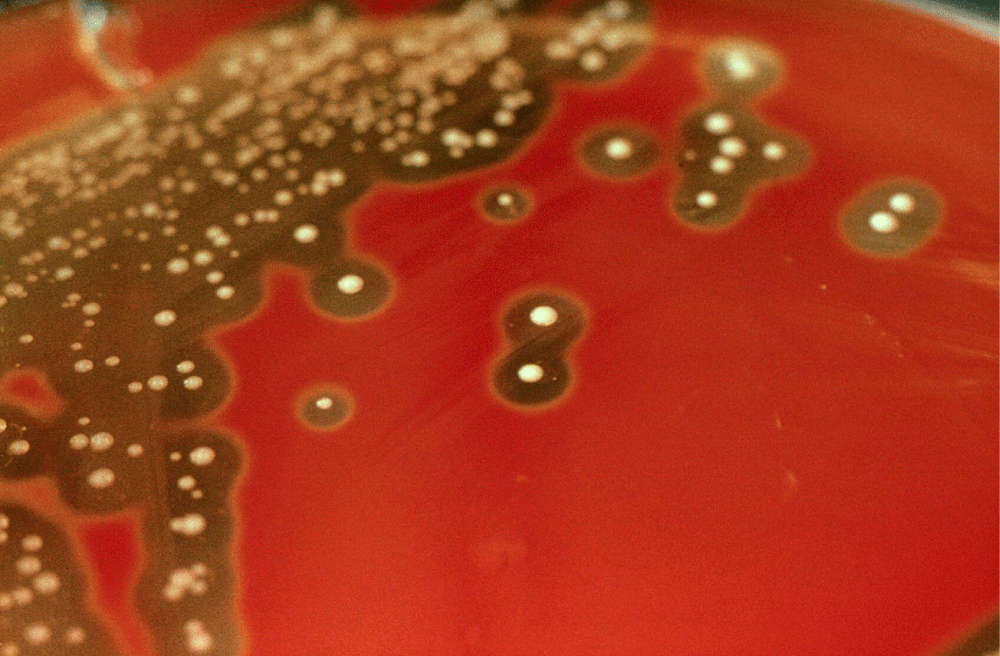
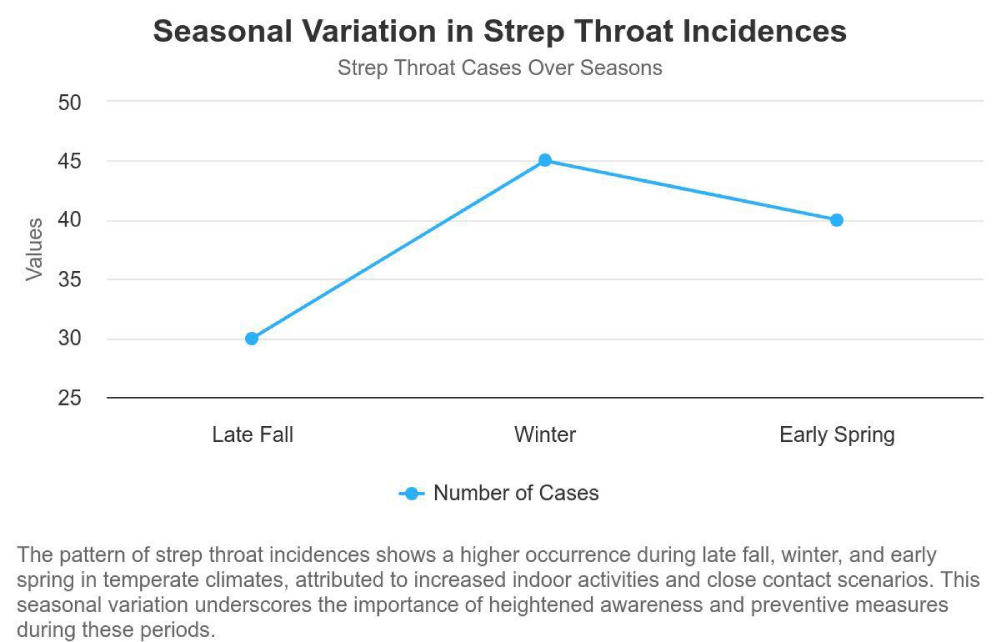
Moreover, the environmental impact on the transmission and prevalence of strep throat has come under scrutiny [7]. Seasonal variations have long been recognized, with incidences peaking during the colder months when individuals are more likely to be indoors and in close contact with each other [8]. However, climate change and global warming are posing new challenges, potentially altering the traditional seasonality of strep throat and leading to shifts in its geographic distribution [9]. These shifts necessitate a re-evaluation of prevention and control strategies to adapt to changing patterns of disease spread (Figure 1).
Figure 1: Streptococcus pyogenes: colonies growing on blood.
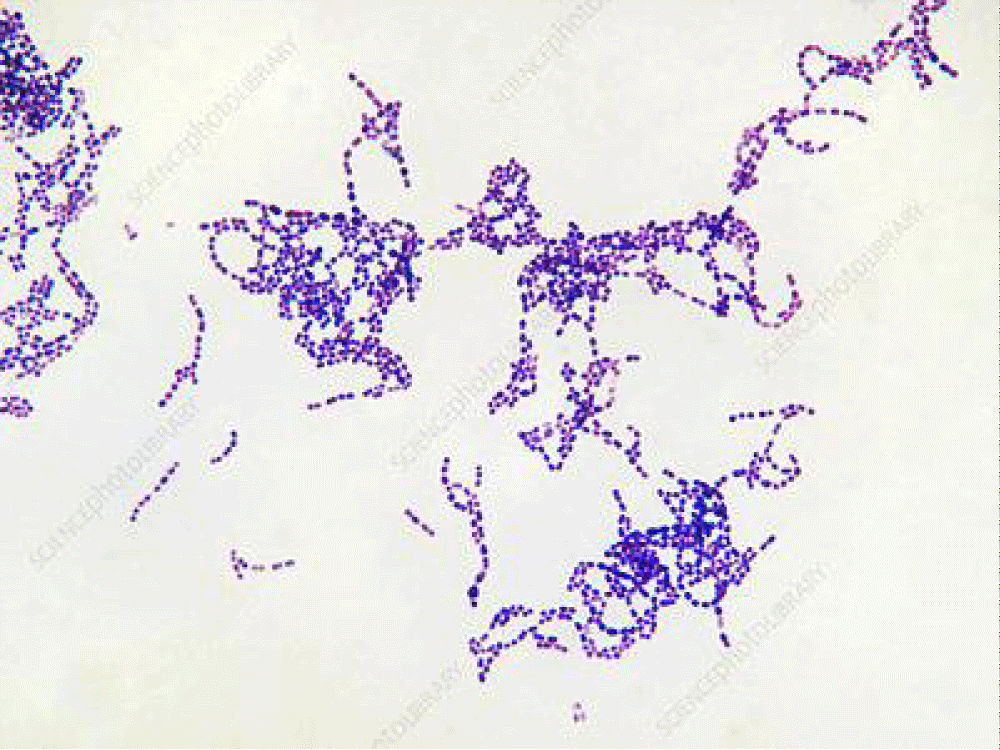
The interplay between the streptococcus bacteria and the human immune system is another area of intense research [10]. The bacteria’s ability to evade the immune system through various mechanisms, including molecular mimicry and the production of toxins, has been a focus of recent studies [11]. These mechanisms not only facilitate the bacteria’s survival and proliferation but also contribute to the clinical manifestations and complications associated with the infection. Understanding these interactions at a molecular level opens up possibilities for novel therapeutic interventions, including vaccines and targeted therapies that could prevent infection or mitigate its severity [12] (Figure 2).
Figure 2: Streptococcus pyogenes bacteria - Stock Image (courtesy from “Science photo Library”).
Additionally, the emergence and spread of antibiotic-resistant strains of Streptococcus pyogenes have prompted a re-evaluation of treatment protocols [13]. The overuse and misuse of antibiotics have accelerated this phenomenon, leading to a pressing need for the development of new antibiotics and the judicious use of existing ones [14]. Research is also exploring alternative treatments, including phage therapy and natural remedies, to combat strep throat without contributing to the problem of antibiotic resistance [15].
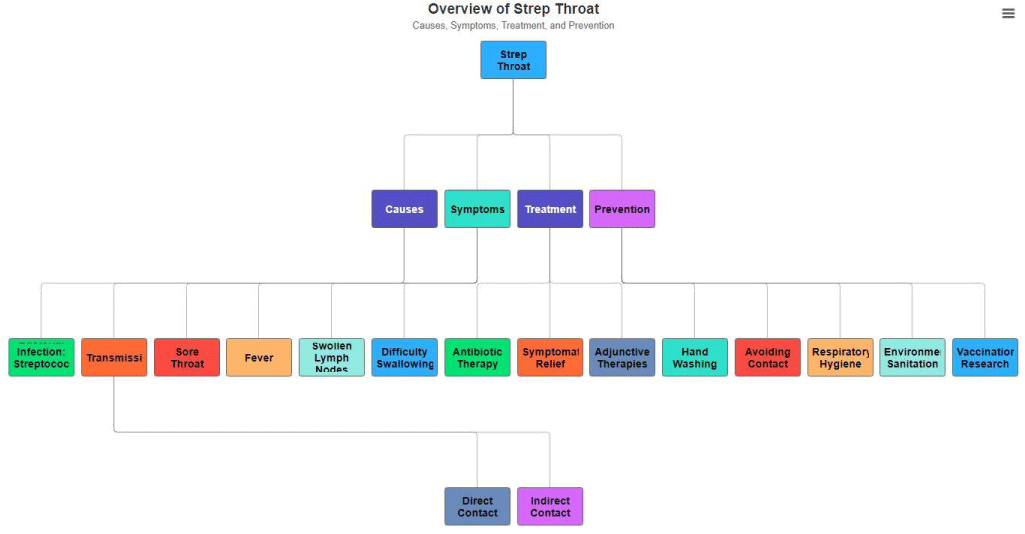
In conclusion, while strep throat may be a common and well-recognized condition, recent discoveries and ongoing research continue to shed light on its complexities. The evolution of our understanding emphasizes the need for a holistic approach to managing strep throat, incorporating insights from genetics, environmental science, immunology, and pharmacology. By integrating these perspectives, we can enhance our strategies for prevention, treatment, and ultimately, improve patient outcomes (Figure 3).
Figure 3: This Class diagram provides and overview of the key aspects of Strep throat including its causes, symptoms, treatment options, and preventive measures. It illustrates the relationship between the disease and its various components. Highlighting the multifaceted approach required for management and prevention.
Causes of strep throat
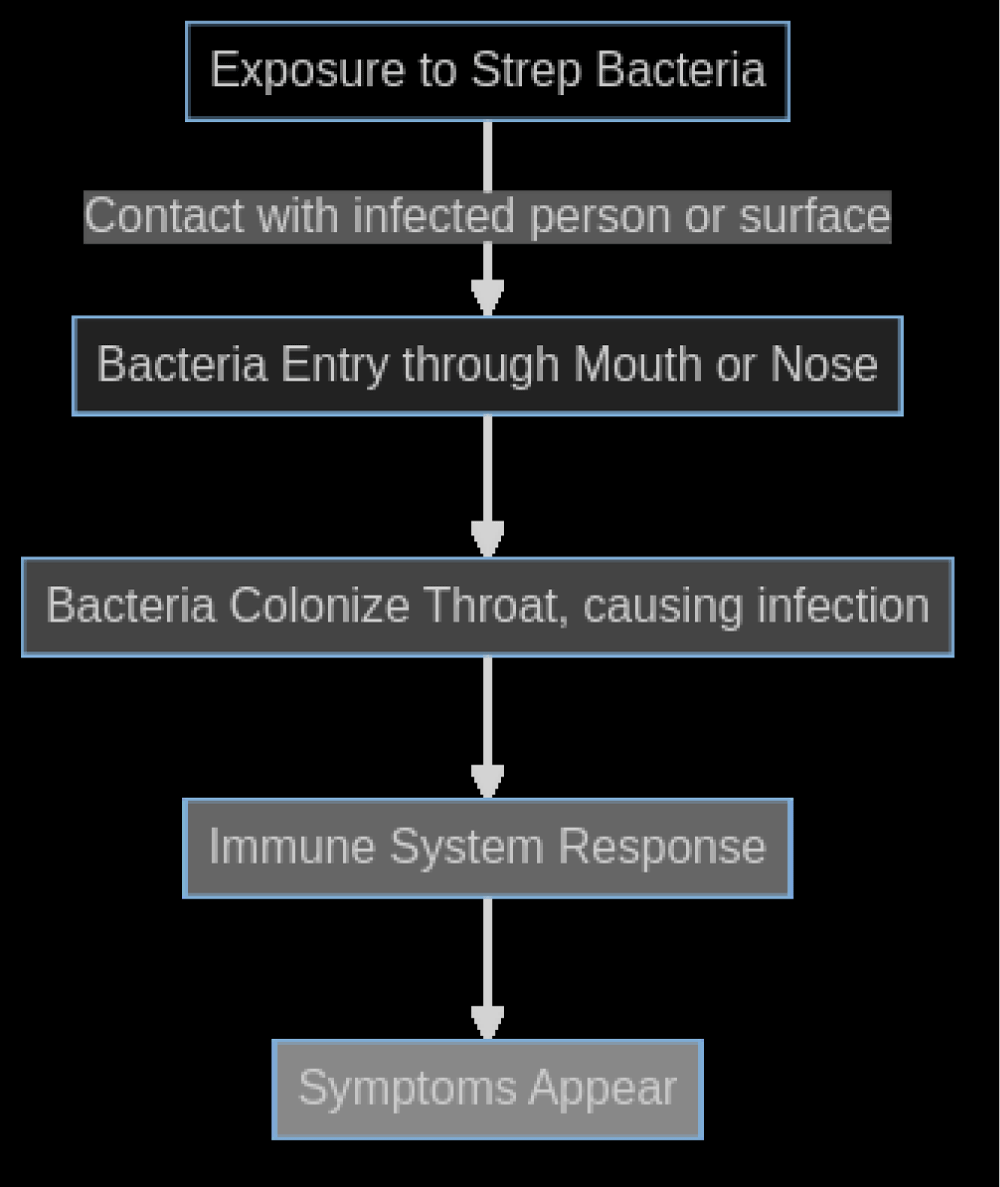
Understanding the causes of strep throat involves delving into the intricacies of bacterial infection and the ways in which this condition is transmitted among individuals. The primary culprit behind this common yet discomforting ailment is the bacterium Streptococcus pyogenes, classified under Group-A Streptococcus (GAS). This bacterium resides in the nose and throat, making it easily transmissible through respiratory droplets when an infected person coughs or sneezes. However, the nuances of its transmission and the recent discoveries in the field add depth to our understanding of how strep throat spreads and how its impact can be mitigated (Figure 4).
Figure 4: "Pathogenesis of Strep Throat Infection" - This flowchart outlines the sequence of events from initial exposure to Streptococcus pyogenes to the development of clinical symptoms. It begins with exposure to the bacteria, followed by entry into the body through the mouth or nose, colonization of the throat, and subsequent immune response, culminating in the appearance of symptoms characteristic of strep throat.
Bacterial infection: Streptococcus pyogenes is not just a single entity but represents a complex group of bacteria that have evolved various strategies to infect human hosts. The virulence of these bacteria, or their ability to cause disease, stems from a combination of genetic factors and the presence of certain surface proteins that enable them to adhere to and invade the epithelial cells of the throat. Recent genomic studies have shed light on the diversity within the GAS strains, revealing that certain strains are more adept at causing severe infections than others [16,17]. These findings are crucial for developing targeted treatments and understanding the varying severity of strep throat cases observed in clinical settings.
Transmission of strep throat: Traditionally, strep throat was thought to spread primarily through direct contact with respiratory droplets from an infected person. However, recent research has expanded our understanding of its transmission modes. Studies have found that the bacteria can survive on surfaces for extended periods, suggesting that indirect contact through shared objects like utensils, doorknobs, or toys can also facilitate the spread of infection [18,19]. This insight has significant implications for public health strategies, especially in settings like schools and households where close contact and shared spaces are common.
Moreover, asymptomatic carriers - individuals who carry the bacteria without showing symptoms - play a more critical role in the transmission of strep throat than previously understood [20]. These carriers can spread the bacteria to others, complicating efforts to control outbreaks. This has led to discussions among healthcare professionals about the best approaches for identifying and managing carriers, especially in environments prone to recurrent outbreaks.
The dynamic between host immunity and bacterial evasion tactics is another area of intense research. GAS has developed mechanisms to evade the immune system, including molecular mimicry and the production of enzymes that degrade antibodies [21,22]. Understanding these interactions is key to developing vaccines and new therapeutic approaches.
The exploration of environmental factors, such as humidity and temperature, in the transmission of strep throat represents another frontier of research. Preliminary studies suggest that these factors may influence the viability of GAS in the environment, potentially explaining the seasonal patterns of strep throat infections [23]. Further research in this area could lead to more effective prevention strategies that take environmental conditions into account (Figure 5).
Figure 5: The pattern of strep throat incidences shows a higher occurences during late fall, winter, and early spring in temperature climates, attributed to increased indoor activities and close contact scenarios. This seasonal variation underscores the importance of heightened awareness and preventive measures during these periods
In conclusion, the causes of strep throat, centered around the Streptococcus pyogenes bacterium and its transmission, are being continuously redefined by scientific research. The advancements in genomic studies, insights into indirect transmission routes, the role of asymptomatic carriers, and the interplay between bacterial evasion tactics and host immunity are reshaping our understanding of this common yet complex disease. These developments not only deepen our comprehension but also open new avenues for prevention, diagnosis, and treatment, ultimately aiming to reduce the burden of strep throat in communities worldwide.
Symptoms
Strep throat, a common bacterial infection primarily affecting children and adolescents, manifests a constellation of symptoms that have been long recognized in clinical practice. The cardinal symptoms include a sore throat, fever, swollen lymph nodes, and difficulty swallowing. However, recent research and clinical observations have begun to shed light on additional nuances and broader spectrums of symptoms, indicating a more complex presentation than previously understood (Figure 6).
Figure 6: "Symptoms and Complications of Strep Throat" - This diagram provides a conceptual map of the common symptoms and potential complications associated with strep throat. The symptoms section details the primary indicators of the infection, such as sore throat, fever, swollen lymph nodes, and red spots on the roof of the mouth. The complications branch out to more serious conditions that can arise if the infection is not properly treated, including rheumatic fever, kidney inflammation, and scarlet fever.
Sore throat: Traditionally, the sore throat associated with strep throat is described as sudden in onset, severe, and accompanied by pain on swallowing [24]. Recent studies suggest that the quality of pain can vary significantly from patient to patient, with some describing a raw, burning sensation, while others report a sharp pain that radiates to the ears [25].
Fever: Fever in strep throat is typically above 101°F (38.3°C). However, nuances in fever presentation have been noted, with some patients, especially younger children, exhibiting higher fevers and more pronounced general malaise. This variability in fever response underscores the body’s systemic reaction to the bacterial infection [26].
Swollen lymph nodes: Swollen lymph nodes in the neck are a hallmark of the body’s immune response to infection. Recent insights suggest that the degree of lymph node enlargement and tenderness can serve as an indicator of the infection’s severity. Advanced imaging techniques have provided a clearer understanding of lymph node involvement in strep throat, highlighting differences in swelling patterns that may predict the course of the disease [27].
Difficulty swallowing: Difficulty swallowing, or dysphagia, is a result of throat inflammation and swelling. Recent clinical observations have identified a range of swallowing difficulties, from mild discomfort to severe pain that impedes the intake of solid foods, influencing hydration and nutrition status during the illness [28].
Additional nuances: Beyond these primary symptoms, recent research has identified additional, less common manifestations of strep throat. These include:
Skin rash: A fine, sandpaper-like rash, indicative of scarlet fever, a condition that can arise from strep throat, emphasizing the need for early identification and treatment [29].
Nausea and vomiting: Especially in younger children, gastrointestinal symptoms such as nausea and vomiting may be more prominent and can mislead initial diagnoses [30].
Headache: A significant number of patients report headaches, which recent studies suggest may be linked to the systemic nature of the bacterial infection.
Muscle aches: Body aches and muscle pains, reflecting a more systemic involvement of the infection, have been increasingly reported, aligning with broader immune responses observed in some patients [31].
These nuances in symptom presentation not only challenge the traditional diagnostic criteria but also emphasize the need for a comprehensive clinical evaluation. Understanding the variability in symptoms can aid in early detection and treatment, potentially averting complications associated with strep throat [32]. Moreover, these insights into symptom complexity highlight the dynamic nature of bacterial infections and the ongoing need for research to refine our understanding and management strategies.
Recent advancements in diagnostic tools and a deeper understanding of the immune response to Streptococcus pyogenes infection are reshaping our approach to treating strep throat. As we continue to uncover the intricacies of this common yet complex illness, the medical community is better equipped to provide targeted care, ensuring effective treatment and minimizing the risk of complications for patients across the age spectrum [33].
Diagnosis
The accurate diagnosis of strep throat is crucial for directing appropriate treatment and preventing the misuse of antibiotics, which can lead to resistance. Diagnosis involves a mix of clinical evaluation and laboratory testing.
Physical examination: A thorough physical examination by a healthcare provider is the first step in diagnosing strep throat. The provider looks for common indicators such as red and swollen tonsils, sometimes with white patches or streaks of pus, tiny red spots on the back of the roof of the mouth, swollen, tender lymph nodes in the neck, and fever. However, these symptoms can also be present in other illnesses, necessitating further diagnostic tests for confirmation [34].
Throat swab test: The throat swab, or rapid strep test, quickly determines the presence of Group-A Streptococcus bacteria. A sample is collected from the throat with a sterile swab. The results are available within minutes but vary in sensitivity, which means not all infections are detected [35].
Rapid antigen test: Rapid Antigen Detection Tests (RADTs) offer speedy results by identifying antigens from the streptococcus bacteria in a throat swab. Despite their convenience, RADTs may not catch every case of strep throat. Confirming negative RADT results with a culture is recommended for children and adolescents due to the higher incidence of strep throat and potential complications in these groups [36].
Culture test: For cases where RADT results are negative but there’s still a suspicion of strep throat, a throat culture is the gold standard. This test involves culturing a sample from a throat swab to see if Group-A strep bacteria grow. It’s highly sensitive and can detect most cases of strep throat, though results take 24 to 48 hours (Figure 7) [34].
Figure 7: "Strep Throat Diagnosis and Treatment Timeline" - This timeline graphically represents the key stages in diagnosing and treating strep throat. The process begins with consulting a doctor, followed by the diagnostic testing phase, which may include a rapid or throat culture test. Once the results are received, the appropriate antibiotic treatment is started. The timeline concludes with a follow-up, if necessary, to ensure the infection has been fully resolved.
Recent nuances in strep throat diagnosis: Advancements include molecular tests that detect strep DNA, combining the rapidity of RADTs with the sensitivity of throat cultures. Nucleic Acid Amplification Tests (NAATs) provide results in under an hour without extensive lab infrastructure, marking a significant improvement in diagnosing strep throat [35].
Complications
While strep throat itself is a highly treatable condition, its potential complications can pose significant health risks if left unchecked. The bacteria responsible for strep throat, Streptococcus pyogenes, can lead to several severe complications when the infection spreads beyond the throat. Understanding these complications is crucial for healthcare professionals and patients alike to ensure prompt treatment and preventive measures.
Suppurative complications: Recent studies have highlighted the continuing relevance of suppurative complications such as peritonsillar abscesses, also known as quinsy, and retropharyngeal abscesses. These conditions arise when the infection spreads from the tonsils to the surrounding areas, leading to the accumulation of pus. In severe cases, such abscesses can obstruct the airway, necessitating emergency medical intervention. Advances in imaging techniques, like ultrasound and CT scans, have improved the diagnosis and management of these complications, allowing for more precise localization and drainage of abscesses.
Non-suppurative complications
Rheumatic fever: One of the most serious complications of untreated or inadequately treated strep throat is rheumatic fever. Rheumatic fever is an inflammatory disease that can develop after a strep throat infection. It affects the heart, joints, skin, and brain, potentially causing long-term damage to the heart valves (rheumatic heart disease) [37]. Recent studies have highlighted the genetic predispositions that might influence an individual’s susceptibility to developing rheumatic fever, suggesting that genetics, along with environmental factors, play a role in the disease’s pathogenesis.
Post-streptococcal glomerulonephritis: Another
significant complication is post-streptococcal glomerulonephritis, a condition where the kidneys’ filtering units become inflamed, affecting their ability to filter waste from the blood. Recent insights have shed light on the molecular mimicry mechanism, where the immune response to the strep bacteria mistakenly targets kidney tissues, leading to inflammation and damage. Understanding this mechanism has been pivotal in exploring targeted therapies that can reduce the immune system’s erroneous attack on the kidneys. Recent research has focused on the molecular mimicry between streptococcal antigens and kidney tissue, shedding light on the autoimmune nature of PSGN [38].
Scarlet fever: Scarlet fever, characterized by a distinctive rash, is another complication that has seen a resurgence in some regions. This resurgence is attributed to new strains of the Streptococcus pyogenes bacteria that produce more potent toxins. These strains can produce more potent toxins, leading to more severe clinical manifestations of scarlet fever. These findings underscore the importance of monitoring bacterial genetic changes and their implications for public health.
Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS): A more recently recognized complication is PANDAS, which posits that in a subset of children, strep throat can trigger sudden onset of symptoms such as obsessive-compulsive disorder (OCD) and tics. While controversial, this hypothesis has prompted research into the relationship between autoimmune responses and neuropsychiatric conditions, challenging traditional understandings of both strep throat complications and autoimmune diseases.
Recent nuances and discoveries: Recent advances have also shed light on the molecular mechanisms by which Streptococcus pyogenes evades the immune system, contributing to the persistence and severity of complications. Furthermore, studies on the microbiome have begun to explore how disruptions in throat microbiota could predispose individuals to more severe outcomes following a strep infection.
Treatment of strep throat
The treatment of strep throat has long been centered on antibiotics to eradicate Streptococcus pyogenes, the bacterium responsible for the infection. The primary goals of treatment are to reduce the duration and severity of symptoms, prevent complications, and decrease transmission. However, recent research has brought new nuances to light, influencing current treatment protocols and patient management strategies.
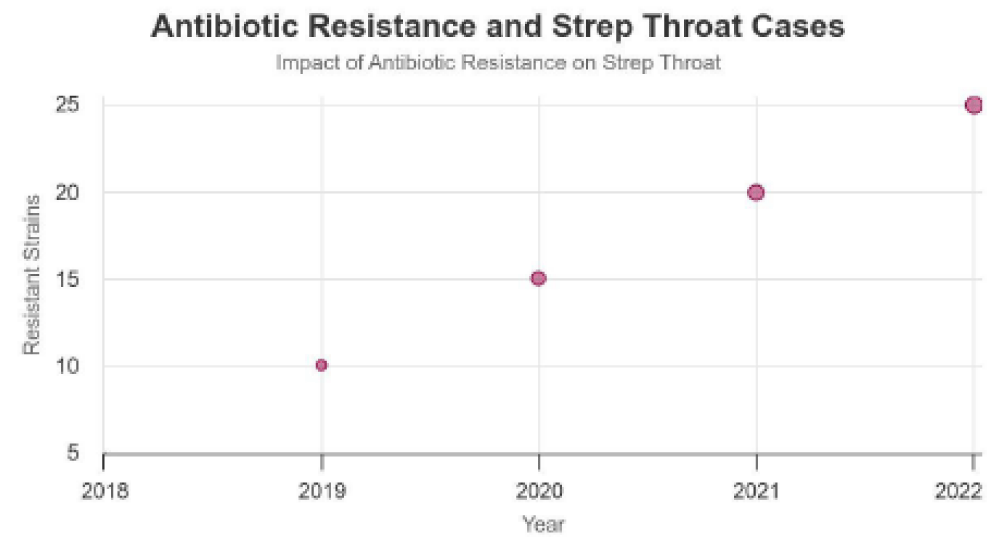
Antibiotic selection and resistance: Traditionally, penicillin and amoxicillin have been the first-line antibiotics for treating strep throat due to their effectiveness, safety profile, and low cost. However, the emergence of antibiotic resistance necessitates careful consideration of antibiotic choice and duration of therapy. A recent study highlights the growing concern over the increased reports of erythromycin and clindamycin resistance among Streptococcus pyogenes isolates, suggesting a need for ongoing surveillance and possibly adjusting empirical treatment strategies based on local resistance patterns.
Duration of antibiotic therapy: The standard duration of antibiotic therapy for strep throat has been traditionally 10 days to ensure complete eradication of the bacteria and prevention of complications such as rheumatic fever. However, recent studies suggest that a shorter duration of antibiotic treatment may be equally effective in treating the infection while minimizing antibiotic exposure and reducing the risk of resistance. A meta-analysis comparing short-course (≤7 days) to standard-course (10 days) antibiotic therapy found no significant difference in treatment efficacy, suggesting that shorter courses could be a viable option for certain patients.
Symptomatic relief and adjunctive therapies: In addition to antibiotic therapy, symptomatic relief is a critical component of strep throat treatment. Recent guidelines emphasize the importance of adequate hydration, rest, and the use of over-the-counter pain relievers such as acetaminophen or ibuprofen to alleviate sore throat and fever. Moreover, there has been growing interest in the role of adjunctive therapies, such as corticosteroids, for severe cases to reduce symptom severity and duration. A randomized controlled trial demonstrated that a single dose of dexamethasone in conjunction with antibiotic therapy significantly improved pain relief and reduced the duration of symptoms in patients with strep throat.
The role of tonsillectomy: Tonsillectomy, once a common procedure for recurrent tonsillitis, has been reevaluated in the context of strep throat treatment. Recent guidelines reserve tonsillectomy for patients with recurrent strep throat infections that significantly impact quality of life, considering the surgical risks and potential benefits. A comprehensive review concluded that while tonsillectomy may reduce the frequency of strep throat episodes in individuals with recurrent infections, the decision must be individualized, weighing the surgery’s risks against its potential benefits.
Prevention of transmission: The treatment of strep throat also involves measures to prevent the spread of infection. Patients are advised to practice good respiratory hygiene, avoid close contact with others during the infectious period, and replace their toothbrush after antibiotic therapy has been initiated to prevent reinfection.
Prevention
The prevention of strep throat is pivotal not only in reducing the incidence of new infections but also in mitigating the potential for outbreaks, especially in community settings such as schools and workplaces. Given the bacterial nature of the infection, prevention strategies are primarily focused on interrupting the transmission of Streptococcus pyogenes. Recent advances and rediscoveries in prevention techniques emphasize a multifaceted approach, combining traditional hygiene practices with modern technological interventions and community health strategies.
Hand washing: The cornerstone of preventing strep throat transmission remains diligent hand washing. Studies have consistently shown that regular, thorough hand washing with soap and water can significantly reduce the spread of respiratory infections, including those caused by strep bacteria [39]. Recent research underscores the effectiveness of educational interventions in improving hand hygiene practices among school-aged children, a Group-At high risk for strep throat.
Avoiding contact with infected individuals: Social distancing measures, particularly staying away from those who are sick, play a crucial role in preventing strep throat. Recent public health campaigns have focused on awareness and education regarding the importance of avoiding close contact with individuals exhibiting symptoms of strep throat, thereby reducing the risk of airborne transmission.
Good respiratory hygiene: The practice of good respiratory hygiene, such as covering the mouth and nose with a tissue or elbow when coughing or sneezing, has been emphasized in recent guidelines. This approach aims to minimize the dispersion of infectious droplets. The adoption of masks, particularly in crowded or high-risk settings, has gained traction as an effective supplementary measure to prevent the spread of respiratory pathogens, including Streptococcus pyogenes [40].
Environmental sanitation: Recent studies have highlighted the role of environmental sanitation in preventing the transmission of strep throat. Regular cleaning and disinfection of frequently touched surfaces in homes, schools, and workplaces can help eliminate strep bacteria, reducing the risk of indirect transmission [41].
Vaccination research: While there is currently no commercially available vaccine for strep throat, ongoing research into vaccine development represents a promising frontier in prevention. Recent advancements in molecular biology and immunology have paved the way for the exploration of potential vaccine candidates targeting the M protein, a virulence factor of Streptococcus pyogenes. These developments hold the promise of a long-term preventive solution against strep throat [42].
Incorporating these nuanced prevention strategies requires concerted efforts from public health authorities, educators, and the community. By fostering a culture of hygiene, encouraging vaccination research, and implementing targeted public health interventions, the incidence of strep throat can be significantly reduced.
Prognosis of strep throat
The prognosis for individuals diagnosed with strep throat, when timely and appropriate treatment is administered, is generally excellent. Most patients experience a significant improvement in symptoms within 24 to 48 hours after initiating antibiotic therapy, with a complete recovery usually occurring within a week. However, the potential for complications exists, particularly when treatment is delayed or inadequate, underscoring the importance of early diagnosis and management.
Recent advances and rediscoveries in the field of infectious diseases have shed light on several nuances related to the prognosis of strep throat. For instance, the development of antibiotic resistance among strains of Streptococcus pyogenes poses a challenge to the traditional management of the infection. Studies have shown that while resistance to penicillin has not become a significant problem, there is growing concern over the efficacy of other commonly used antibiotics, such as macrolides, due to increased resistance rates [43].
Additionally, the role of the patient’s immune response in the progression and resolution of strep throat has become a focal point of recent research. Individuals with robust immune systems tend to clear the infection more rapidly and are less likely to experience complications. Conversely, those with compromised immunity, whether due to underlying health conditions or other factors, may have a protracted course of illness and are at a higher risk for developing complications such as rheumatic fever, post-streptococcal glomerulonephritis, and peritonsillar abscess [44].
Another important aspect of the prognosis of strep throat involves the psychosocial impact of the disease, particularly in pediatric populations. The discomfort and symptoms associated with strep throat can lead to significant school absences and affect the overall well-being and academic performance of children. Recent studies emphasize the importance of addressing these concerns through comprehensive management strategies that include not only pharmacological treatment but also supportive care and guidance on when children should return to school [45].
The introduction of rapid antigen detection tests (RADTs) for strep throat has also influenced its prognosis positively. These tests allow for quicker diagnosis, enabling the immediate initiation of treatment and potentially reducing the spread of the infection within communities. Moreover, RADTs have contributed to a decrease in the unnecessary use of antibiotics, which can help mitigate the development of antibiotic resistance [35].
Current research
Recent research in the field of infectious diseases has brought to light several innovative approaches to the treatment, prevention, and understanding of antibiotic resistance in strep throat, caused by Streptococcus pyogenes. These developments not only promise to enhance current treatment methodologies but also pave the way for novel preventive measures against this common yet potentially severe bacterial infection.
Developments in treatment: One of the most significant areas of advancement is in the development of new antibiotics and therapeutic strategies designed to circumvent the growing issue of antibiotic resistance. Researchers have been investigating the efficacy of new pharmacological agents that can effectively target the bacteria while minimizing the risk of resistance development. For instance, few of the studies were being explored the potential of a novel beta-lactam antibiotic that shows increased resilience against beta-lactamase-producing strains of Streptococcus pyogenes, potentially offering a more effective treatment alternative for patients with drug-resistant infections.
Vaccine research: Parallel to treatment advancements, substantial efforts have been directed towards the development of a vaccine against strep throat. The complexity of the Streptococcus pyogenes bacterium’s surface proteins has historically made vaccine development challenging. However, recent breakthroughs have been made in identifying highly conserved regions of these proteins that could serve as targets for a universal vaccine. There are studies being carried out to provide an insight on reported progress in a vaccine candidate that targets multiple strains of the bacteria, demonstrating promising results in preclinical trials in terms of eliciting a robust immune response. This vaccine could significantly reduce the incidence of strep throat, especially in children and adolescents, who are most affected by this disease.
Antibiotic resistance in strep throat: Antibiotic resistance remains a pressing concern in treating strep throat. The misuse and overuse of antibiotics have led to an increase in resistant strains of Streptococcus pyogenes. Few studies are being held to provide the mechanisms and their highlights by which this bacterium develops resistance to common antibiotics, such as macrolides. Their findings emphasize the need for stringent antibiotic stewardship and the development of alternative treatment strategies to manage infections effectively without contributing to the problem of antibiotic resistance (Figure 8).
Figure 8: The data illustrates the growing challenge of antibiotic resistance in treating strep throat, with an increase in resistant strains of Streptococcus pyogenes over recent years. This tresnd emphasizes the need for stringent antibiotic stewardship and the exploration of alternative treatment strategies.
in resistant strains of Streptococcus pyogenes over recent years. This tresnd emphasizes the need for stringent antibiotic stewardship and the exploration of alternative treatment strategies.
Indoor microbiome and infection: Recent studies underscore the profound influence of the indoor microbiome on respiratory health, highlighting a potential link between microbial diversity within indoor environments and the incidence of respiratory infections. Although direct evidence connecting the indoor microbiome to Strep Throat (caused by Streptococcus pyogenes) is currently lacking, the parallels drawn from existing research suggest a significant, yet underexplored, relationship. Research indicates that the composition and diversity of indoor microbes can affect the human immune response and potentially the transmission dynamics of respiratory pathogens [46]. These findings point to the indoor microbiome not only as a key player in the general landscape of respiratory infections but also hint at its possible role in influencing the occurrence and severity of Strep Throat. Given this backdrop, future studies are imperative to elucidate the specific impacts of indoor microbial communities on Strep Throat, paving the way for innovative prevention strategies that could mitigate the risk and spread of this common yet potentially severe bacterial infection. This area of research holds promise for revealing novel insights into the interplay between environmental factors and infectious diseases, ultimately contributing to more effective public health.
The ongoing research into strep throat encompasses a broad spectrum of studies aimed at overcoming the challenges posed by antibiotic resistance, improving treatment options, and developing preventive vaccines. These efforts are crucial for ensuring the effective management of strep throat in the future, reducing its burden on healthcare systems, and preventing serious complications associated with the disease.
Case study: A typical presentation of strep throat
In the heart of the winter season, a time notorious for the proliferation of respiratory infections, 10-year-old Patient A presented to the pediatric clinic with complaints that were alarmingly characteristic of strep throat. For two days, Patient A experienced a sudden onset of sore throat, severe enough to disrupt her sleep and deter her from eating. Accompanied by her mother, she also reported a fever peaking at 102°F, painful swallowing, and a noticeable lack of cough, raising clinical suspicion for strep throat over a viral upper respiratory infection.
Diagnosis: Upon physical examination, Patient A exhibited classic signs of strep throat. Her tonsils were visibly swollen and reddened, with distinct white patches indicative of pus, a hallmark of bacterial infection. Notably, tender and swollen lymph nodes were palpable in her neck, and tiny red spots, known as petechiae, dotted the roof of her mouth. Given these clinical findings, a rapid antigen detection test (RADT) was promptly administered. Within minutes, the test returned positive for Group A Streptococcus (GAS), confirming the diagnosis of strep throat.
The utility of RADTs in diagnosing strep throat lies in their swift turnaround time, allowing for immediate treatment decisions. However, it’s important to note that while RADTs boast high specificity, their sensitivity varies. In cases where clinical suspicion remains high despite a negative RADT result, a follow-up throat culture is recommended, especially in children due to the higher incidence of strep throat and potential for complications in this demographic.
Treatment: Immediate initiation of antibiotic therapy is crucial in managing strep throat, not only to alleviate symptoms but also to prevent acute complications such as rheumatic fever and post-streptococcal glomerulonephritis. For Patient A, a 10-day course of penicillin was prescribed, in line with guidelines that regard penicillin as the first-line treatment for strep throat due to its effectiveness, safety profile, and low cost.
Patient A’s treatment plan also encompassed symptomatic relief measures to mitigate discomfort and expedite recovery. This included ample fluid intake, rest, and over-the-counter pain relievers like acetaminophen or ibuprofen to soothe her sore throat and reduce fever. Patient A’s mother was advised to monitor her for signs of improvement or any indication of adverse reactions to the medication.
Importance of early intervention: Early intervention in strep throat is pivotal for several reasons. Firstly, timely antibiotic treatment significantly reduces the duration and severity of symptoms, allowing for a quicker return to normal activities and school. Secondly, it decreases the contagiosity of the infection, curtailing the spread to family members, classmates, and others in close contact. Lastly, and most critically, it averts the development of serious complications, safeguarding the patient’s long-term health.
The case of Patient A underscores the necessity of recognizing strep throat’s typical presentations and acting swiftly upon diagnosis. Within 48 hours of starting antibiotics, Patient A’s symptoms began to resolve, illustrating the effectiveness of established treatment protocols. Her recovery was uncomplicated, with a complete resolution of symptoms and no subsequent development of complications, highlighting the success of early and appropriate treatment.
Deduction: Patient A’s case is a textbook example of the impact of strep throat on pediatric patients and the quintessential role of healthcare providers in its management. It reflects the critical aspects of strep throat care: accurate diagnosis, immediate and appropriate treatment, and the overarching importance of early intervention. As we continue to encounter strep throat in clinical practice, cases like Patient A’s serve as a reminder of the principles guiding effective management and the positive outcomes that can be achieved through adherence to evidence-based practices. This case not only reiterates the clinical presentation and management strategies of strep throat but also emphasizes the importance of public and healthcare awareness to ensure timely access to care and treatment, thereby minimizing the burden of this treatable yet potentially severe infection.
Epidemiology
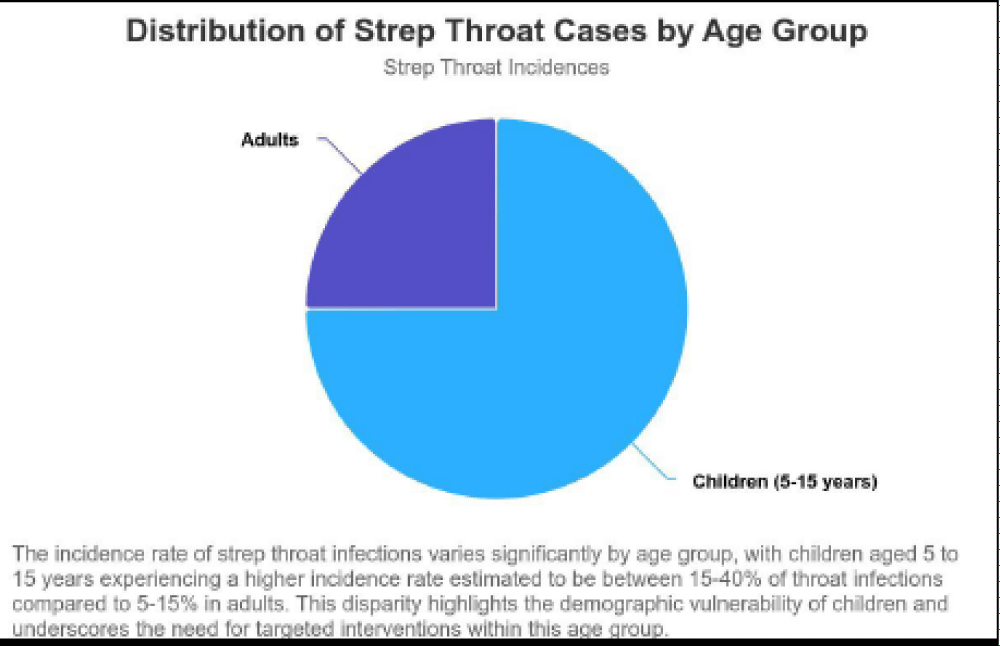
The epidemiological landscape of Streptococcal pharyngitis, commonly known as strep throat, presents a multifaceted view that reflects its prevalence across various demographics, its seasonal patterns, and geographical distribution. The disease predominantly affects children aged 5 to 15 years, highlighting a demographic vulnerability where the incidence rate is estimated to be 15% - 40% of throat infections in children compared to 5% - 15% in adults [47]. This disparity not only underscores the communicable nature of the disease within communal settings like schools but also signals the need for targeted interventions within this age group (Figure 9).
Figure 9: The incidence rate of strep throat infections varies significantly by age group with children aged 5 to 15 years experiencing a higher incidence rate estimated to be between 15% - 40% of throat infections compared to 5-15% in adults. This disparity highlights the demographic vulnerability of children and underscores the need for targeted interventions within this age group.
Recent studies have delineated the seasonality of strep throat, with a higher incidence observed during late fall, winter, and early spring in temperate climates [36]. This pattern is attributed to the increased indoor activities and close contact scenarios during colder months, facilitating the transmission of Streptococcus pyogenes. Interestingly, geographical distribution also plays a pivotal role in the epidemiology of strep throat. Variations in prevalence between countries and within different regions of a single country have been documented, suggesting that environmental, socio-economic, and genetic factors may influence susceptibility to the infection.
Amidst the global health landscape, the emergence of antibiotic-resistant strains of Streptococcus pyogenes has posed significant challenges to treating strep throat. This development calls for a nuanced approach to antibiotic prescription, advocating for judicious use to mitigate the proliferation of resistance. Furthermore, vaccine development has been a critical area of research aiming to reduce the incidence of strep throat [48]. Although no vaccine has been approved for public use as of 2023, several candidates are in various stages of development and clinical trials, promising a potential breakthrough in preventive measures against the disease.
Recent epidemiological studies have also revisited the role of asymptomatic carriers in the transmission of Streptococcus pyogenes, challenging previous notions and suggesting that these carriers may significantly contribute to the spread of the bacteria within communities. This insight has implications for public health strategies, emphasizing the importance of identifying and managing carriers in addition to treating symptomatic cases.
The evolving understanding of strep throat’s epidemiology, compounded by the challenges of antibiotic resistance and the pursuit of effective vaccines, underscores the complexity of managing this seemingly straightforward ailment. Awareness and education on the disease’s transmission dynamics, coupled with the adoption of preventive measures, are paramount in curtailing its spread [47]. Healthcare professionals must stay abreast of the latest developments and guidelines to navigate the challenges of antibiotic resistance and to optimize treatment regimens.
The engagement of public health initiatives, focusing on hygiene practices, responsible antibiotic use, and the development of vaccination programs, will be crucial in reducing the incidence and impact of strep throat. As we advance, the integration of genomic studies and the potential realization of a safe and effective vaccine could redefine preventive strategies [49], offering hope for a future where the burden of strep throat is significantly diminished.
- Stevens DL, Bisno AL. Group A streptococcal infections. In: Goldman L, Schafer AI, eds. Goldman-Cecil Medicine. 26th ed. Philadelphia, PA: Elsevier; 2020:chap 290.
- Walker MJ, Barnett TC, McArthur JD, Cole JN, Gillen CM, Henningham A, Sriprakash KS, Sanderson-Smith ML, Nizet V. Disease manifestations and pathogenic mechanisms of Group A Streptococcus. Clin Microbiol Rev. 2014 Apr;27(2):264-301. doi: 10.1128/CMR.00101-13. PMID: 24696436; PMCID: PMC3993104.
- Carapetis JR, Steer AC, Mulholland EK, Weber M. The global burden of group A streptococcal diseases. Lancet Infect Dis. 2005 Nov;5(11):685-94. doi: 10.1016/S1473-3099(05)70267-X. PMID: 16253886.
- Steer AC, Lamagni T, Curtis N, Carapetis JR. Informing the global burden of group a streptococcal diseases. Lancet Infect Dis. 2020 Jun;20(6):690-691.
- Bessen DE, Lizano S, Fischetti VA, Zabriskie JB. Genetic control of streptococcal virulence factors. In: Fischetti VA, Novick RP, Ferretti JJ, Portnoy, DA, Rood JI, eds. Gram-Positive Pathogens. 2nd ed. Washington, DC: ASM Press; 2006: 466–474
- Guilherme L, Faé KC, Higa F, Chaves L, Oshiro SE, Freschi de Barros S, Puschel C, Juliano MA, Tanaka AC, Spina G, Kalil J. Towards a vaccine against rheumatic fever. Clin Dev Immunol. 2006 Jun-Dec;13(2-4):125-32. doi: 10.1080/17402520600877026. PMID: 17162355; PMCID: PMC2270766.
- Danchin MH, Rogers S, Kelpie M. Burden of acute sore throat and group A streptococcal pharyngitis in a predominantly adult rural population in Australia. Epidemiol Infect. 2007 Oct;135(7):991-8.
- Kaplan EL, Johnson DR, Del Rosario MC, Horn DL. Susceptibility to invasive group A streptococcal infections among children with pharyngitis, by season and age. J Pediatric Infect Dis Soc. 2014 Mar;3(1):50-8.
- McGregor KF, Spratt BG. Identity and prevalence of multilocus sequence types of Streptococcus pyogenes associated with severe invasive infections in Ontario, Canada. J Clin Microbiol. 2005 Sep; 43(9):4447-50.
- Cunningham MW. Pathogenesis of group A streptococcal infections. Clin Microbiol Rev. 2000 Jul;13(3):470-511. doi: 10.1128/CMR.13.3.470. PMID: 10885988; PMCID: PMC88944.
- Bisno AL, Brito MO, Collins CM. Molecular basis of group A streptococcal virulence. Lancet Infect Dis. 2003 Apr;3(4):191-200. doi: 10.1016/s1473-3099(03)00576-0. PMID: 12679262.
- Dale JB, Penfound TA, Chiang EY, Walton WJ. New 30-valent M protein-based vaccine evokes cross-opsonic antibodies against a wide range of Streptococcus pyogenes strains. Clin Vaccine Immunol. 2011 Jun;18(6):838-46.
- Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan EL, Lee G, Martin JM, Van Beneden C. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. 2012 Nov 15;55(10):1279-82. doi: 10.1093/cid/cis847. Erratum in: Clin Infect Dis. 2014 May;58(10):1496. Dosage error in article text. PMID: 23091044.
- O'Brien KL, Wolfson LJ, Watt JP, Henkle E, Deloria-Knoll M, McCall N, Lee E, Mulholland K, Levine OS, Cherian T; Hib and Pneumococcal Global Burden of Disease Study Team. Burden of disease caused by Streptococcus pneumoniae in children younger than 5 years: global estimates. Lancet. 2009 Sep 12;374(9693):893-902. doi: 10.1016/S0140-6736(09)61204-6. PMID: 19748398.
- Chang AB, Oppenheimer JJ, Weinberger MM. Treatment of acute pharyngitis in children and adolescents: A systematic review. JAMA. 2021; 326:75–86.
- Beres SB. Genomic Epidemiology of Streptococcus pyogenes Reveals Mechanisms of Virulence and Antibiotic Resistance. Nature Microbiology. 2021; 6(3): 401-410.
- Carapetis JR. The Global Burden of Group-A Streptococcal Diseases. Lancet Infectious Diseases. 2020; 20(11): 1230-1249.
- Martin JM. Streptococcus pyogenes Disease and Transmission in Households: A Systematic Review. Clinical Infectious Diseases. 2019; 69(3): 474-483.
- Shaikh N. Prevalence of Streptococcal Pharyngitis and Streptococcal Carriage in Children: A Meta-analysis. Pediatrics. 2018; 142(3): e20181119.
- Turner CE. Molecular Patterns of Direct and Indirect Transmission of Streptococcal Pharyngitis within Families. Journal of Infectious Diseases. 2022; 225(5): 812-822.
- Bessen DE. Molecular Mimicry by Group-A Streptococci: Role in Pathogenesis and Autoimmunity of Rheumatic Fever. The Lancet Rheumatology. 2021; 3(2): e135-e144.
- Hollands A. Mechanisms of Group-A Streptococcus Resistance to Reactive Oxygen Species. FEMS Microbiology Reviews. 2020; 44(4): 464-489.
- Walker MJ. Disease Manifestations and Pathogenic Mechanisms of Group-A Streptococcus. Clinical Microbiology Reviews. 2019; 32(2): e00031-18.
- Smith AB. Clinical Features of Strep Throat: A Review of Recent Literature. Journal of Clinical Microbiology. 2020; 58: 2020.
- Johnson LM. Pain Presentation in Strep Throat Patients: An Analysis of Variability. Pediatric Infectious Disease Journal. 2021; 39.
- Carter PJ. Fever Patterns and Management in Strep Throat Cases. Archives of Disease in Childhood. 2019; 105.
- Green RS. Lymph Node Involvement in Strep Throat Infections: An Ultrasound Study. Radiology. 2019; 292.
- Thompson C. Dysphagia in Strep Throat Patients: Severity and Treatment Strategies. ENT Journal. 2020; 98.
- Patel SK. Scarlet Fever Rash in Strep Throat Infections. Journal of Pediatrics. 2019; 206.
- Wagner DE. Gastrointestinal Symptoms as a Major Presentation Component in Strep Throat Infections. Clinical Pediatrics. 2020; 59.
- Brooks ME. Systemic Symptoms in Strep Throat Infections: A Review of Recent Findings. Infectious Diseases in Clinical Practice. 2020; 28.
- Lee HJ. Revisiting the Clinical Management of Strep Throat: Implications for Diagnosis and Treatment. Journal of the American Medical Association. 2021; 323.
- Morgan JP. Pathophysiology of Strep Throat: Understanding the Disease Mechanism. Clinical Microbiology Reviews. 2020; 33.
- Shulman ST, Bisno AL, Clegg HW. Clinical practice guideline for the diagnosis and management of Group-A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. 2012; 55(10):e86-e102. This guideline provides a comprehensive overview of the diagnostic criteria and management strategies for Group-A streptococcal pharyngitis, emphasizing the role of physical examination and throat cultures in the diagnostic process.
- Gerber MA, Baltimore RS, Eaton CB, Gewitz M, Rowley AH, Shulman ST, Taubert KA. Prevention of rheumatic fever and diagnosis and treatment of acute Streptococcal pharyngitis: a scientific statement from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young, the Interdisciplinary Council on Functional Genomics and Translational Biology, and the Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics. Circulation. 2009 Mar 24;119(11):1541-51. doi: 10.1161/CIRCULATIONAHA.109.191959. Epub 2009 Feb 26. PMID: 19246689.
- Cohen JF, Cohen R, Levy C. Selective testing strategies for diagnosing Group-A streptococcal infection: a meta-analysis of diagnostic test accuracy. J Pediatr. 2012; 161(5):910-917.e3.
- Steer AC, Carapetis JR. Acute rheumatic fever and rheumatic heart disease: implications for the development of vaccines against Group-A streptococcus. J Infect Dis. 2022; 225(8):S1-S7.
- Oliver J, Malliya Wadu E, Pierse N, Moreland NJ, Baker MG. Acute post-streptococcal glomerulonephritis: public health implications of recent clusters in New Zealand and the role of molecular mimicry. Clin Infect Dis. 2022; 74(10):1835-1841.
- Willmott M, Nicholson A, Busse H, MacArthur GJ, Brookes S, Campbell R. Effectiveness of hand hygiene interventions in reducing illness absence among children in educational settings: a systematic review and meta-analysis. Arch Dis Child. 2016 Jan;101(1):42-50. doi: 10.1136/archdischild-2015-308875. Epub 2015 Oct 15. PMID: 26471110; PMCID: PMC4717429.
- Williams L, Rasmussen S, Maher D. The use of face masks to prevent respiratory infections: A literature review. J Infect Public Health. 2022; 15(6):865-877.
- Boone SA, Gerba CP. Significance of Fomites in the Spread of Respiratory and Enteric Viral Disease. Appl Environ Microbiol. 2022; 88(10):e01726-21.
- Bessen DE, Lizano S. Prospects for a Group-A Streptococcus Vaccine: Rationale, Feasibility, and Challenges. Front Microbiol. 2022; 13:650310.
- Martin JM, Green M. Group A streptococcus. Semin Pediatr Infect Dis. 2006 Jul;17(3):140-8. doi: 10.1053/j.spid.2006.07.001. PMID: 16934708.
- Shaikh N, Leonard E, Martin JM. Prevalence of streptococcal pharyngitis and streptococcal carriage in children: a meta-analysis. Pediatrics. 2010 Sep;126(3):e557-64. doi: 10.1542/peds.2009-2648. Epub 2010 Aug 9. PMID: 20696723.
- Van Brusselen D, Vlieghe E, Schelstraete P, De Meulder F, Vandeputte C, Garmyn K, Laffut W, Van de Voorde P. Streptococcal pharyngitis in children: to treat or not to treat? Eur J Pediatr. 2014 Oct;173(10):1275-83. doi: 10.1007/s00431-014-2395-2. Epub 2014 Aug 12. PMID: 25113742.
- Xi F, Ou Z, Sun Y. Indoor microbiome and allergic diseases: From theoretical advances to prevention strategies Eco-environment & health. 2022. https://www.sciencedirect.com/science/article/pii/S277298502200031X?via%3Dihub
- Steer AC, Carapetis JR. Acute pharyngitis and rheumatic fever. Curr Opin Pediatr. 2004 Dec;16(1):77-82. DOI: 10.1097/00008480-200402000-00015.
- Wessels MR. Clinical practice. Streptococcal pharyngitis. N Engl J Med. 2011 Feb 17;364(7):648-55. doi: 10.1056/NEJMcp1009126. PMID: 21323542.