More Information
Submitted: 08 June 2020 | Approved: 10 August 2020 | Published: 11 August 2020
How to cite this article: Bradish T, Kaushal S, Shakeel M, Ahmad Z. Protecting teeth and gums during rigid endoscopy of the upper aerodigestive tract: Our experience with a disposable, mouldable and rigid thermoplastic mouthguard. Heighpubs Otolaryngol Rhinol. 2020; 4: 018-020.
DOI: 10.29328/journal.hor.1001021
Copyright License: © 2020 Bradish T, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Protecting teeth and gums during rigid endoscopy of the upper aerodigestive tract: Our experience with a disposable, mouldable and rigid thermoplastic mouthguard
Bradish T1, Kaushal S1, Shakeel M1* and Ahmad Z2
1Department of Otolaryngology-Head and Neck Surgery, Aberdeen Royal infirmary, Aberdeen, UK
2Department of Otolaryngology-Head and Neck Surgery, Counties Manukau Health, Manukau Superclinic, 901 Great South Road, Manurewa, Auckland
*Address for Correspondence: Muhammad Shakeel, Consultant ENT / Thyroid Surgeon, Department of Otolaryngology-Head and Neck Surgery, Aberdeen Royal infirmary, Foresterhill Road, Aberdeen, AB252ZN, UK, Email: [email protected]
Direct rigid pharyngoscopy, laryngoscopy and oesophagoscopy are very common procedures in the Otolaryngology-Head & Neck department, both for diagnostic and therapeutic purposes. The phayngoscopes, laryngoscopes and oesophagoscopes are solid straight metal instruments to facilitate examination and passage of instruments through them. The process of pharyngo-laryngo-oesophagoscopy invariably involves some contact with the upper dentition resulting in some pressure over the teeth and jaw when suspension laryngoscopy is carried out.
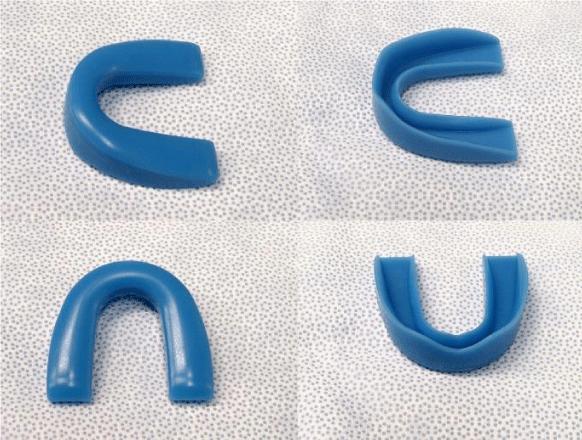
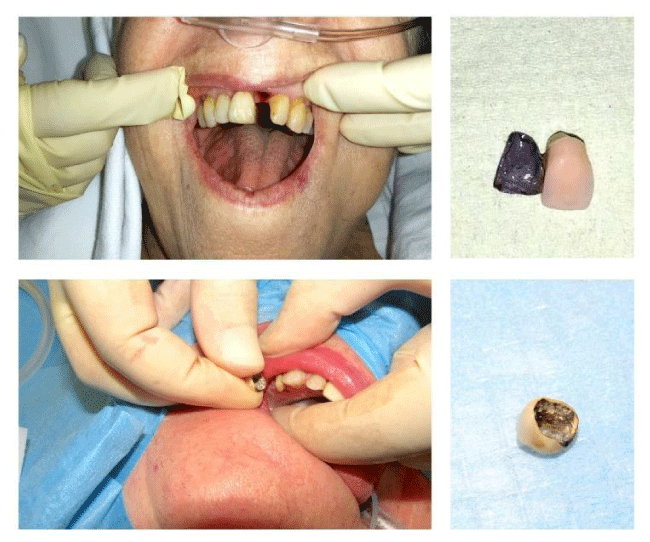
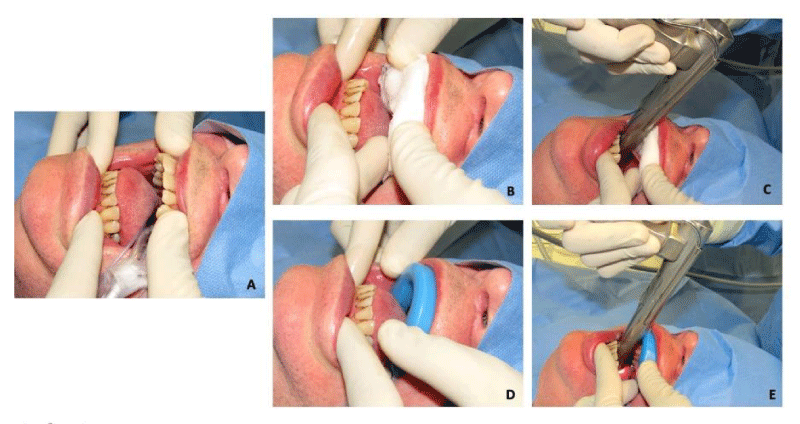
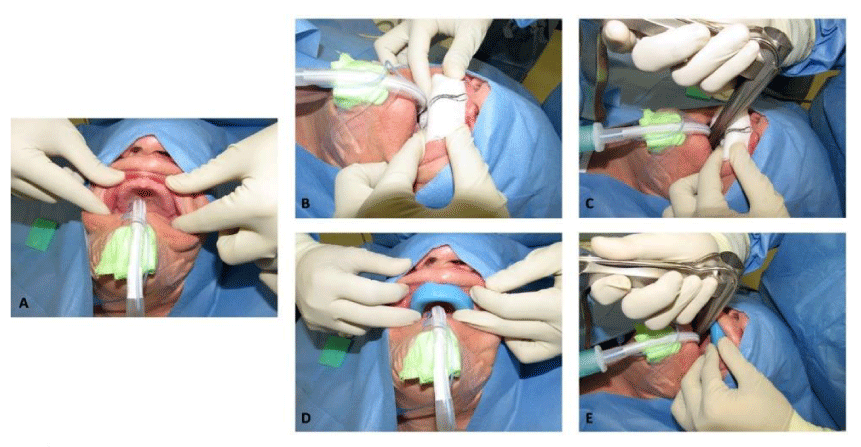
Dental damage should be included on the consent form for any patient undergoing pharyngo-laryngo-oesophagoscopy as dental injury following laryngoscopy has been reported to be as high as 25% [1]. The soft, commercially available, single use dental guards are commonly used during rigid endoscopy of the upper aerodigestive tract (Figure 1). These guards may protect against teeth chipping but dental trauma (Figure 2) is not an uncommon occurrence because of inadequate pressure distribution and sometimes slipping of these traditional dental guards during endoscopy. Some surgeons prefer to use 2 wet swabs during rigid endoscopy [2] for protection of gums and teeth which does not adequately protect against chipping of the sharp teeth (Figures 3,4). Unfortunately, excessive pressure on the gums can lead to significant ulceration and similarly tongue can be bruised if caught between teeth and endoscope (Figure 5).
Figure 1: Commercially available preformed, flexible teeth guard made of silicone elastomer.
Figure 2: Dental trauma during rigid laryngoscopy despite using the soft silicone teeth guard.
Figure 3: Demonstration of prominent teeth protection (A) during rigid laryngoscopy using wet swabs (B & C) and by using silicone teeth guard (D & E). Lips are protected by the non-dominant hand (C & E).
Figure 4: Demonstration of protection of edentulous upper gums (A) during rigid laryngoscopy using wet swabs (B & C) and by using the silicone guard (D & E). It is very difficult to keep the guard in place during the procedure (E).
Figure 5: Ulceration of the upper gums because of excessive pressure of the rigid laryngoscope despite covering the gums with wet swabs (A & B). Also, visible is the bruised tongue (C).
For patients who undergo frequent laryngoscopies (e.g. recurrent respiratory papillomatosis) they are advised to visit their dentist to have a custom fitted mouth guard made which can be used for every sitting of surgery [3]. This has the benefit of spreading the load across multiple teeth but is costly and not financially viable in patients undergoing only one or two aerodigestive intervention or in patients for whom diagnosis and commencing treatment is time critical.
In this article we describe using Aquaplast (Patterson Medical) thermoplastic splinting material as a quick and cost-effective way of making a custom fit mouth guard to minimise dental damage during rigid endoscopy. We also describe other important steps to minimise dental injury.
Technique
Preoperative: The best way of minimizing dental trauma is still to minimize excessive contact pressure with teeth [2]. Adequate dental assessment through examination and history prior to any aerodigestive rigid endoscopy is therefore essential to identify the at-risk patient or teeth.
Patient factors associated with increased risk of dental injury are [4]:
• Prominent incisors
• Mallampati grade 3/4
• Inter incision distance <5cm
• Limited head/neck movement
• Receding mandible
• Obesity
• Previous dental restorations or orthodontic treatment
• Wobbly teeth
Operative: The patient should be correctly positioned on the table to maximize view, this has traditionally been the “Sniffing the morning air” position involving flexion of the cervical spine and gentle extension of the head at the atlanto-axial joint. However recent studies have shown that it should be individualized for the patient and that aerodigestive examination should be performed on a table with a movable headrest to allow for dynamic changes in position intraoperatively based on patient anatomy [5].
Materials
Aquaplast (Patterson Medical) is a latex free thermoplastic polymer in sheet form which becomes soft and mouldable when heated before setting hard again when returning to room temperature.
Procedure (video)
Video: Procedure.
The authors recommend the 1.6 mm thick aquaplast-T sheet. This comes in large sheets of 46 x 61 cm so an individual piece of approximately 10 x 10 cm should be cut preoperatively (Figure 6). This can be further trimmed to individual patient specifications prior to softening. Although multiple colours are available the authors recommend the white sheet as it turns from white to clear to white on heating and cooling giving an indicator to the malleability of the material. The sheet should be put into water or saline with a temperature of approx. 70 degree Celsius and observed until it becomes clear, this takes approximately 35 seconds. It should then be removed and allowed to partially cool. Prior to molding to the patient’s dentition, the temperature of the sheet should be checked on the back of the operating surgeon’s hand or the inside of the wrist to check that the temperature is suitable.
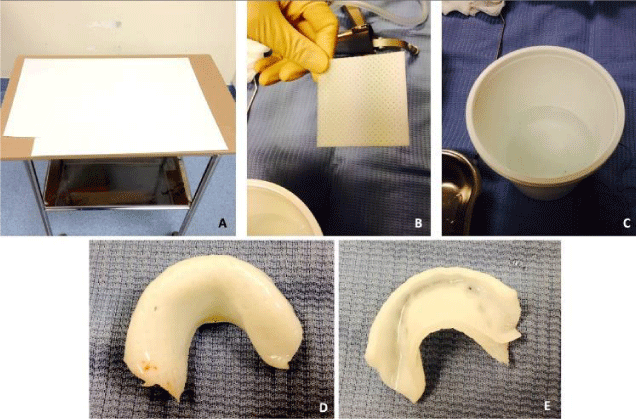
Figure 6: Demonstration of creating a rigid thermoplastic teeth guard: Aquaplast sheet (A); a square piece of aquaplast (B); Hot water tub (C) Teeth guard ready to use showing extension onto the hard palate for diversion of force away from the teeth (D & E).
The sheet can then be folded in half to double the thickness with the folded edge on the side of the labial sulcus to minimize sharp edges in this location. Cooling of this product takes approximately 1-2 minutes and the surgeon should apply gentle pressure to mould the product during this time. The process can be accelerated by using a wet swab with cold saline or water to further cool the product once in place (Figure 7). Once cooled the pharyngo -laryngoscopy or oesophagoscopy can continue. The molded guard can be given to the patient to take home and can be re-used for future procedures if required. If the dentition of the patient has since changed the material can be re-softened and re-moulded to the new dentition (Figure 8).
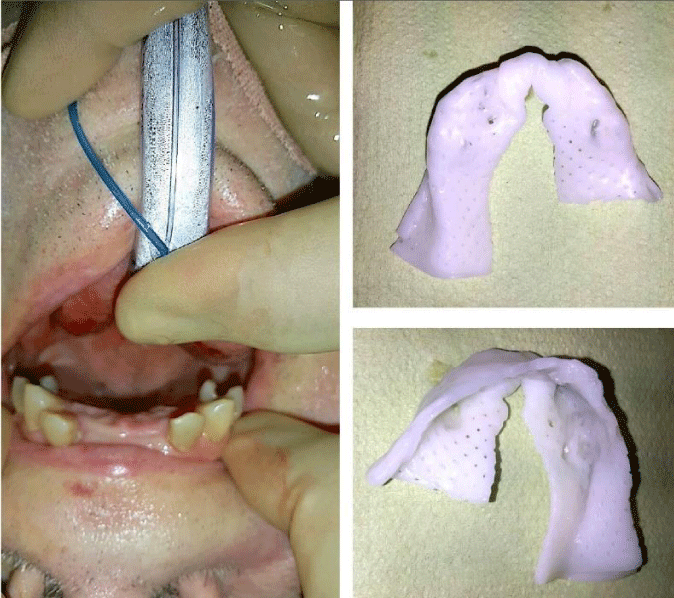
Figure 7: The softened aquaplast sheet is double folded (A), placed onto the teeth, moulded and cooled by wet swab while maintaining digital pressure (B) till the guard is hard (C).
Figure 8: In patients with missing teeth the aquaplast sheet can be moulded according to dentition thereby transferring the laryngoscope pressure uniformly to the teeth and minimising risk.
Dental injury is a well-documented risk associated with rigid endoscopy of the upper aerodigestive tract. Through careful planning, procedural skill and patient positioning this can be minimised and every effort should be made to avoid using the teeth as a fulcrum while carrying out the rigid laryngoscopy [2]. In addition to wet swabs and silicone teeth guard a number of other mouth guards have been suggested including the “Boil and Bite” mouth guard2 which we believe because of its soft nature still does not protect the teeth from breaking. In patients with prominent upper teeth, a 1-2 millimeter reduction in the inter incisor distance because of the teeth guard proposed by Talmon and Gilbey [6] can contribute to difficult access and increases the risk of dental trauma. Formation and application of a thermoplastic mouthguard as suggested by Domanski, et al. [7] spreads the laryngoscope-related pressure uniformly onto the teeth. We employ extending the teeth guard onto the hard palate which has helped us greatly to minimise dental trauma during rigid endoscopy. The senior author (ZA) has successfully used this mouth guard in his practice for more than 15 years without any side effects to the patients and staff. We have no hesitation to recommend use of this mouth guard in every patient undergoing aerodigestive endoscopy.
- Mourão J, Neto J, Luís C, Moreno C, Barbosa J, et al. Dental injury after conventional direct laryngoscopy: A prospective observational study. Anaesthesia. 2013; 68: 1059–1065. PubMed: https://pubmed.ncbi.nlm.nih.gov/24047290/
- Crossland GJ, Pfleiderer AG. 'Boil and Bite' mouth guards for direct laryngoscopy. Clin Otolaryngol. 2007; 32: 121‐122.
- Olson GT, Moreano EH, Arcuri MR, Hoffman HT. Dental protection during rigid endoscopy. Laryngoscope. 1995; 105: 662‐663.
- Abeysundara L, Creedon A, Soltanifar D. Dental knowledge for anaesthetists. BJA Educ. 2016;16: 362–368.
- Myatra S. Optimal position for laryngoscopy - Time for individualization? J Anaesthesiol Clin Pharmacol. 2019; 35: 289–291. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6748012/
- Talmon Y, Gilbey P. Self-made tooth guard using Turbocast™. J Laryngol Otology. 2001; 115: 209-211.
- Domanski M, Lee P, Sadeghi N. Cost-effective dental protection during rigid endoscopy. Laryngoscope. 2011; 121: 2590‐2591. PubMed: https://pubmed.ncbi.nlm.nih.gov/22109757/